What is the most important information I should know about ibandronate?
You should not use ibandronate if you have severe kidney disease or low levels of calcium in your blood.
Do not take an ibandronate tablet if you have problems with your esophagus, or if you cannot sit upright or stand for at least 60 minutes after taking the tablet.
Ibandronate tablets can cause serious problems in the stomach or esophagus. Stop taking ibandronate and call your doctor at once if you have chest pain, new or worsening heartburn, or pain when swallowing.
Also call your doctor if you have muscle spasms, numbness or tingling (in hands and feet or around the mouth), new or unusual hip pain, or severe pain in your joints, bones, or muscles.
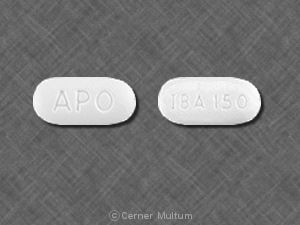
What is ibandronate?
Ibandronate is a bisphosphonate (bis FOS fo nayt) medicine that alters bone formation and breakdown in the body. This can slow bone loss and may help prevent bone fractures.
Ibandronate is used to treat or prevent osteoporosis in women after menopause.
Ibandronate may also be used for purposes not listed in this medication guide.
What should I discuss with my healthcare provider before using ibandronate?
You should not use ibandronate if you are allergic to it, or if you have:
- severe kidney disease; or
- low blood levels of calcium (hypocalcemia).
Do not take an ibandronate tablet if you have problems with your esophagus, or if you cannot sit upright or stand for at least 60 minutes. Ibandronate can cause serious problems in the stomach or esophagus. You must stay upright for at least 1 full hour after taking this medicine.
To make sure ibandronate is safe for you, tell your doctor if you have ever had:
- trouble swallowing;
- problems with your stomach or digestion;
- hypocalcemia;
- a dental problem (you may need a dental exam before you begin using ibandronate);
- kidney disease; or
- any condition that makes it hard for your body to absorb nutrients from food (malabsorption).
In rare cases, this medicine may cause bone loss (osteonecrosis) in the jaw. Symptoms include jaw pain or numbness, red or swollen gums, loose teeth, or slow healing after dental work. The longer you use ibandronate, the more likely you are to develop this condition.
Osteonecrosis of the jaw may be more likely if you have cancer or received chemotherapy, radiation, or steroids. Other risk factors include blood clotting disorders, anemia (low red blood cells), and a pre existing dental problem.
Talk with your doctor about the risks and benefits of using this medication.
It is not known whether ibandronate will harm an unborn baby. Tell your doctor if you are pregnant or plan to become pregnant.
It is not known whether ibandronate passes into breast milk or if it could harm a nursing baby. Tell your doctor if you are breast-feeding a baby.
How should I use ibandronate?
Follow all directions on your prescription label. Do not use this medicine in larger or smaller amounts or for longer than recommended.
Ibandronate tablets are taken once per month. Ibandronate injection is given into a vein through an IV once every 3 months.
Ibandronate tablets can be taken at home, but a healthcare provider must give the ibandronate injection.
Take the ibandronate tablet first thing in the morning, at least 60 minutes before you eat or drink anything or take any other medicine. Take the medicine on the same day each month and always first thing in the morning.
Take the ibandronate tablet with a full glass (6 to 8 ounces) of plain water. Do not use coffee, tea, soda, juice, or mineral water. Do not eat or drink anything other than plain water.
Do not crush, chew, or suck on an ibandronate tablet. Swallow it whole.
For at least 60 minutes (1 full hour) after taking an ibandronate tablet:
-
Do not lie down or recline.
-
Do not take any other medicine including vitamins, calcium, or antacids.
Pay special attention to your dental hygiene while using ibandronate. Brush and floss your teeth regularly. If you need to have any dental work (especially surgery), tell the dentist ahead of time that you are using ibandronate.
Ibandronate is only part of a complete program of treatment that may also include diet changes, exercise, bone mineral density testing, and taking calcium and vitamin supplements. Follow your doctor's instructions very closely.
Store at room temperature away from moisture and heat.
Your doctor will determine how long to treat you with this medicine. Ibandronate is often given for only 3 to 5 years.
What happens if I miss a dose?
Ibandronate tablets: If you forget to take a tablet first thing in the morning on your scheduled day, do not take it later in the day. Wait until the next morning to take the missed dose. Then return to your regular monthly schedule on your chosen dose day. If your next scheduled dose is less than 7 days away, wait until then and skip the missed dose. Do not take two (2) doses in one week.
Ibandronate injections: Call your doctor for instructions if you miss an appointment for your injection.
What happens if I overdose?
For oral ibandronate: Drink a full glass of milk and seek emergency medical attention or call the Poison Help line at 1-800-222-1222. Do not make yourself vomit and do not lie down.
Since ibandronate injections are given by a healthcare professional in a medical setting, an overdose is unlikely to occur.
What should I avoid while taking ibandronate?
Avoid taking any other medicines for at least 60 minutes after taking ibandronate. This includes vitamins, calcium, and antacids. Some medicines can make it harder for your body to absorb ibandronate.
Avoid smoking, or try to quit. Smoking can reduce your bone mineral density, making fractures more likely.
Avoid drinking large amounts of alcohol. Heavy drinking can also cause bone loss.
What are the possible side effects of ibandronate?
Get emergency medical help if you have signs of an allergic reaction: hives; wheezing, difficult breathing; swelling of your face, lips, tongue, or throat.
Stop using ibandronate and call your doctor at once if you have:
- chest pain, new or worsening heartburn;
- difficulty or pain when swallowing;
- pain or burning under the ribs or in the back;
- severe heartburn, burning pain in your upper stomach, or coughing up blood;
- new or unusual pain in your thigh or hip;
- jaw pain, numbness, or swelling;
- severe joint, bone, or muscle pain; or
-
low calcium levels --muscle spasms or contractions, numbness or tingly feeling (around your mouth, or in your fingers and toes).
Common side effects may include:
- heartburn, stomach pain, diarrhea;
- back pain, bone pain, muscle or joint pain;
- pain in your arms or legs;
- headache; or
- fever, chills, tiredness, flu-like symptoms.
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
What other drugs will affect ibandronate?
Tell your doctor about all your current medicines and any you start or stop using, especially:
- aspirin; or
-
NSAIDs (nonsteroidal anti-inflammatory drugs) --ibuprofen (Advil, Motrin), naproxen (Aleve), celecoxib, diclofenac, indomethacin, meloxicam, and others.
This list is not complete. Other drugs may interact with ibandronate, including prescription and over-the-counter medicines, vitamins, and herbal products. Not all possible interactions are listed in this medication guide. Talk with your doctor about the best dosing schedule for your other medicines.
Where can I get more information?
Your pharmacist can provide more information about ibandronate.
Remember, keep this and all other medicines out of the reach of children, never share your medicines with others, and use this medication only for the indication prescribed.
Every effort has been made to ensure that the information provided by Cerner Multum, Inc. ('Multum') is accurate, up-to-date, and complete, but no guarantee is made to that effect. Drug information contained herein may be time sensitive. Multum information has been compiled for use by healthcare practitioners and consumers in the United States and therefore Multum does not warrant that uses outside of the United States are appropriate, unless specifically indicated otherwise. Multum's drug information does not endorse drugs, diagnose patients or recommend therapy. Multum's drug information is an informational resource designed to assist licensed healthcare practitioners in caring for their patients and/or to serve consumers viewing this service as a supplement to, and not a substitute for, the expertise, skill, knowledge and judgment of healthcare practitioners. The absence of a warning for a given drug or drug combination in no way should be construed to indicate that the drug or drug combination is safe, effective or appropriate for any given patient. Multum does not assume any responsibility for any aspect of healthcare administered with the aid of information Multum provides. The information contained herein is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. If you have questions about the drugs you are taking, check with your doctor, nurse or pharmacist.
Copyright 1996-2018 Cerner Multum, Inc. Version: 11.03. Revision date: 11/21/2017.