Hemodialysis
Treatment Overview
Chronic kidney disease and acute kidney injury(also known as acute renal failure) cause the kidneys to lose their ability to filter and remove waste and extra fluid from the body. Hemodialysis is a process that uses a man-made membrane (dialyzer) to:
- Remove wastes, such as urea, from the blood.
- Restore the proper balance of electrolytes in the blood.
- Eliminate extra fluid from the body.
For hemodialysis, you are connected to a filter (dialyzer) by tubes attached to your blood vessels. Your blood is slowly pumped from your body into the dialyzer, where waste products and extra fluid are removed. The filtered blood is then pumped back into your body.
There are different types of hemodialysis. Talk about these with your doctor to decide which one might be best for you.
- In-center hemodialysis. You go to a hospital or a dialysis center. Hemodialysis usually is done 3 days a week and takes 3 to 5 hours a day.
- Home hemodialysis. After you are trained, you do your dialysis treatments at home. Hemodialysis is usually done 3 days a week (or every other day). Discuss with your doctor how long each session needs to be. A session could be as long as 6 hours, which may help you feel better.
- Daily home hemodialysis. After you are trained, you do your dialysis treatments at home. Hemodialysis is done 5 to 7 days a week. Each session takes about 3 hours.
- Nocturnal home hemodialysis. After you are trained, you do your dialysis treatments at home. Hemodialysis is done 3 to 7 nights a week. Each session is done overnight (about 6 to 8 hours).
Before treatments can begin, your doctor will need to create a site where the blood can flow in and out of your body during the dialysis sessions. This is called the dialysis access. The type of dialysis access you have will depend in part on how quickly you need to begin hemodialysis.
There are different types of access for hemodialysis:
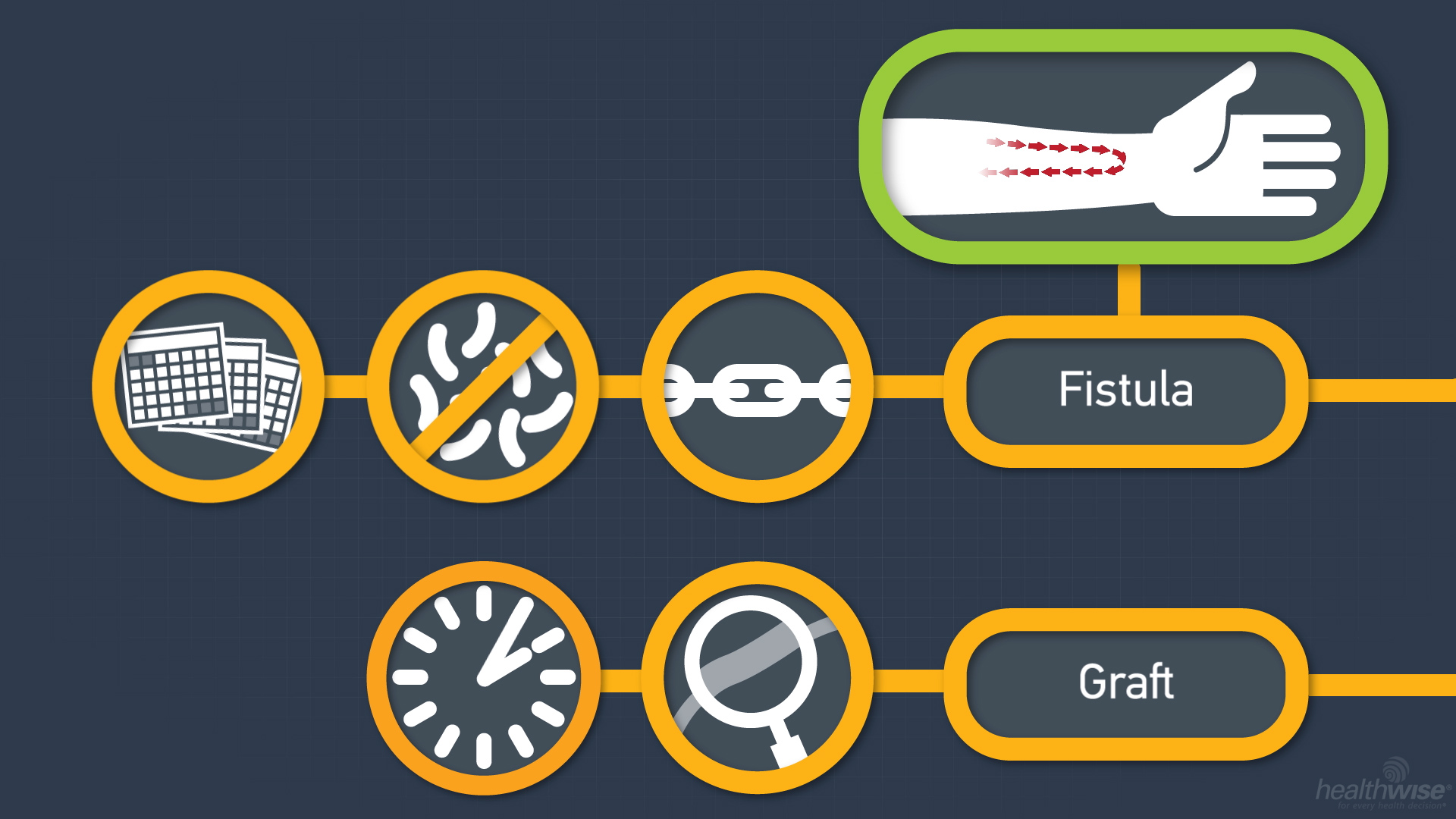
- Fistula. A fistula is created by connecting an artery to a vein in your lower arm. A fistula allows repeated access for each dialysis session. It may take several months for the fistula to form. A fistula may not clot as easily as other dialysis access methods. A fistula is the most effective dialysis access and the most durable. Complications include infection at the site of access and clot formation (thrombosis).
- Graft. A vascular access that uses a synthetic tube implanted under the skin in your arm (graft) may be used if you have very small veins. The tube becomes an artificial vein that can be used repeatedly for needle placement and blood access during hemodialysis. A graft does not need to develop as a fistula does, so a graft can sometimes be used as soon as 1 week after placement. Compared with fistulas, grafts tend to have more problems with clotting or infection and need to be replaced sooner. A polytetrafluoroethylene (PTFE or Gore-Tex) graft is the most common type used for hemodialysis.
- Venous catheter. A tube, or catheter, may be used temporarily if you have not had time to get a permanent access. The catheter is usually placed in a vein in the neck, chest, or groin. Because it can clog and become infected, this type of catheter is not routinely used for permanent access. But if you need to start hemodialysis right away, a catheter may be used until your permanent access is ready.
Hemodialysis for acute kidney injury may be done daily until kidney function returns.
Choosing between treatment with hemodialysis or peritoneal dialysis is based on your lifestyle, other medical conditions, and body size and shape. Talk to your doctor about which type would be best for you.
What To Expect
About once a month, you will have blood tests to make sure you are getting the right amount of hemodialysis. These tests are done to help find out how well hemodialysis is working. Your weight before and after each session will be recorded, as will the length of time it takes to complete the dialysis session. If you have hemodialysis at home, you will need to keep records of your weight before and after each session and the length of each session.
Why It Is Done
Hemodialysis is often started after symptoms or complications of kidney failure develop. Symptoms or complications may include:
- Signs of uremic syndrome, such as nausea, vomiting, loss of appetite, and fatigue.
- High levels of potassium in the blood (hyperkalemia).
- Signs of the kidneys' inability to rid the body of daily excess fluid intake, such as swelling.
- High levels of acid in the blood (acidosis).
- Inflammation of the sac that surrounds the heart (pericarditis).
Hemodialysis is sometimes used when acute kidney injury develops. Dialysis is always used with extra caution in people who have acute kidney injury, because dialysis can sometimes cause low blood pressure, irregular heart rhythms (arrhythmias), and other problems that can make acute kidney injury worse.
How Well It Works
Hemodialysis may improve your quality of life and increase your life expectancy. But hemodialysis provides only about 10% of normal kidney function. It does not reverse chronic kidney disease or kidney failure.
Dialysis has not been shown to reverse or shorten the course of acute kidney injury. But it may be used when fluid and electrolyte problems are causing severe symptoms or other problems. Some people who develop acute kidney injury stay dependent on hemodialysis and will go on to develop kidney failure.
Risks
Most complications that occur during dialysis can be prevented or easily managed if you are monitored carefully during each dialysis session. Possible complications may include:
- Low blood pressure (hypotension). This is the most common complication of hemodialysis.
- Muscle cramps.
- Irregular heartbeat (arrhythmia).
- Nausea, vomiting, headache, or confusion (dialysis disequilibrium).
- Infection, especially if a central venous access catheter is used for hemodialysis.
- Blood clot (thrombus) formation in the venous access catheter.
- Technical complications, such as trapped air (embolus) in the dialysis tube.
Long-term complications of dialysis may include:
- Inadequate filtering of waste products (hemodialysis inadequacy).
- Blood clot (thrombus) formation in the dialysis graft or fistula.
- Cardiovascular disease (heart disease, blood vessel disease, or stroke).
What To Think About
If you have severe chronic kidney disease and you have not yet developed kidney failure, talk with your doctor about which type of dialysis might work best for you.
People who have widely fluctuating blood pressure when they receive hemodialysis (hemodynamic instability) may not be able to continue with treatment. They may be switched to peritoneal dialysis.
Many people first receive dialysis while waiting for a kidney transplant. Some people may have to receive dialysis again if the kidney transplant fails.
Current as of: March 15, 2018