Coronary Artery Disease
Topic Overview

What is coronary artery disease?
Coronary artery disease is the most common type of heart disease. It's also the number one killer of both men and women in the United States.
When you have it, your heart muscle doesn't get enough blood. This can lead to serious problems, including heart attack.
It can be a shock to find out that you have coronary artery disease. Many people only find out when they have a heart attack. Whether or not you have had a heart attack, there are many things you can do to slow coronary artery disease and reduce your risk of future problems.
What causes coronary artery disease?
Coronary artery disease is caused by hardening of the arteries, or atherosclerosis. This means that fatty deposits called plaque (say "plak") build up inside the arteries. Arteries are the blood vessels that carry oxygen-rich blood throughout your body.
Atherosclerosis can affect any arteries in the body. When it occurs in the ones that supply blood to the heart (the coronary arteries), it is called coronary artery disease.
When plaque builds up in the coronary arteries, the heart may not get the blood it needs to work well. Over time, this can weaken or damage the heart. If a plaque tears, the body tries to fix the tear by forming a blood clot around it. The clot can block blood flow to the heart and cause a heart attack.
What are the symptoms?
Symptoms can happen when the heart is working harder and needs more oxygen, such as during exercise. Symptoms include:
- Angina (say "ANN-juh-nuh" or "ann-JY-nuh"), which most often is chest pain or discomfort or a strange feeling in the chest.
- Shortness of breath.
- Heart attack. A heart attack is sometimes the first sign of coronary artery disease.
Less common symptoms include a fast heartbeat, feeling sick to your stomach, and increased sweating. Some people don't have any symptoms. In rare cases, a person can have a "silent" heart attack, without symptoms.
How is coronary artery disease diagnosed?
Your doctor will do a physical exam and ask questions about your past health and your risk factors. Risk factors are things that increase the chance that you will have coronary artery disease.
Some common risk factors are being older than 65; smoking; having high cholesterol, high blood pressure, or diabetes; and having heart disease in your family.
If your doctor thinks that you have coronary artery disease, you may have tests to check how well your heart is working. These tests include an electrocardiogram (EKG or ECG), a chest X-ray, an exercise electrocardiogram, and blood tests. You may also have a coronary angiogram to check blood flow to the heart.
How is it treated?
Treatment focuses on lowering your risk for heart attack and stroke and managing your symptoms. Lifestyle changes, medicine, and procedures are used.
- Lifestyle changes include quitting smoking (if you smoke), eating heart-healthy foods, getting regular exercise, staying at a healthy weight, lowering your stress level, and limiting how much alcohol you drink. A cardiac rehab program can help you make these changes.
- Medicines can help you lower high cholesterol and high blood pressure, manage angina, and lower your risk of having a blood clot.
- Procedures that improve blood flow to the heart include angioplasty and bypass surgery.
Health Tools
Health Tools help you make wise health decisions or take action to improve your health.
- Advance Care Planning: Should I Stop Treatment That Prolongs My Life?
- Aspirin: Should I Take Daily Aspirin to Prevent a Heart Attack or Stroke?
- Coronary Artery Disease: Should I Have an Angiogram?
- Coronary Artery Disease: Should I Have Angioplasty for Stable Angina?
- Coronary Artery Disease: Should I Have Bypass Surgery?
- High Blood Pressure: Should I Take Medicine?
- Statins: Should I Take Them to Prevent a Heart Attack or Stroke?
Frequently Asked Questions
|
Learning about coronary artery disease: |
|
|
Being diagnosed: |
|
|
Getting treatment: |
|
|
Preventing coronary artery disease: |
|
|
Living with heart disease: |
|
|
End-of-life issues: |
Cause
Coronary artery disease is caused by hardening of the arteries, or atherosclerosis. This means that fatty deposits called plaque build up inside the arteries. Arteries are the blood vessels that carry oxygen-rich blood throughout your body.
Atherosclerosis can affect any arteries in the body. When it occurs in the arteries that supply blood to the heart (the coronary arteries), it is called coronary artery disease.
When plaque builds up in the coronary arteries, the heart may not get the blood that it needs to work well. This is called ischemia (say "is-KEE-mee-uh"). Ischemia can cause symptoms such as chest pain or pressure. Over time, ischemia can weaken or damage the heart. Sometimes the plaque buildup does not limit blood flow.
If the plaque breaks apart, it can cause a heart attack. A tear or rupture in the plaque tells the body to repair the injured artery lining, much as the body might heal a cut on the skin. A blood clot forms to seal the area. The blood clot can completely block blood flow to the heart muscle and cause a heart attack.
Symptoms
The most common symptoms of coronary artery disease are angina (say "ANN-juh-nuh" or "ann-JY-nuh") and shortness of breath when exercising or doing other vigorous activity. Women are somewhat more likely than men to have other symptoms like nausea and back or jaw pain.
Angina
Angina symptoms include chest pain or pressure or a strange feeling in the chest. This feeling can be in areas other than the chest, such as in the neck or jaw. Angina can be stable or unstable.
- Stable angina means that you can usually predict when your symptoms will happen. You probably know what things cause your angina. For example, you know how much activity usually causes your angina. You also know how to relieve your symptoms.
- Unstable angina means that your symptoms have changed from your typical pattern of stable angina. Your symptoms do not happen at a predictable time. For example, you may feel angina when you are resting. Your symptoms may not go away with rest or nitroglycerin. Unstable angina is an emergency. It may mean that you are having a heart attack.
Silent ischemia
Some people don't have any symptoms. This is called "silent ischemia." In rare cases, you can even have a "silent heart attack," a heart attack without symptoms.
What Increases Your Risk
Things that increase your risk of coronary artery disease are the things that lead to a problem called atherosclerosis, or hardening of the arteries. Atherosclerosis is the starting point for coronary artery disease, peripheral arterial disease, heart attack, and stroke.
Your doctor can help you find out your risk of heart disease, heart attack, and stroke. Knowing your risk is just the beginning for you and your doctor. Knowing your risk can help you and your doctor talk about whether you need to lower your risk. Together, you can decide what treatment is best for you.
Things that increase your risk include:
- High cholesterol.
- High blood pressure.
- Diabetes.
- Smoking.
- A family history of early heart disease. Early heart disease means you have a male family member who was diagnosed before age 55 or a female family member who was diagnosed before age 65.
Your age, sex, and race can also raise your risk. For example, your risk increases as you get older.
To learn how to lower your risk, see Prevention.
When to Call a Doctor
Do not wait if you think you are having a heart attack. Some people aren't sure whether they're having one, or they don't want to bother others, so they wait. But getting help fast can save your life.
Call 911 or other emergency services immediately if you have symptoms of a heart attack or are with someone who has symptoms. Symptoms may include:
- Chest pain or pressure, or a strange feeling in the chest.
- Sweating.
- Shortness of breath.
- Nausea or vomiting.
- Pain, pressure, or a strange feeling in the back, neck, jaw, or upper belly or in one or both shoulders or arms.
- Lightheadedness or sudden weakness.
- A fast or irregular heartbeat.
After you call 911, the operator may tell you to chew 1 adult-strength or 2 to 4 low-dose aspirin. Wait for an ambulance. Do not try to drive yourself. By taking an ambulance, you may be able to start treatment before you arrive at the hospital.
Nitroglycerin. If you typically use nitroglycerin to relieve angina and if one dose of nitroglycerin has not relieved your symptoms within 5 minutes, call 911. Do not wait to call for help.
Call your doctor if:
- Your angina symptoms are different, more frequent, or severe.
Who to see
To see if you are at risk for heart disease, have symptoms of heart disease, or need long-term care for existing heart disease, see your family doctor or internist. For diagnosis of coronary artery disease, you may see a cardiologist. For ongoing care of stable angina, you will likely see your family doctor or an internist. For angioplasty or surgery, you will be referred to an interventional cardiologist or cardiovascular surgeon.
Exams and Tests
Your doctor will do a physical exam and a number of tests to find out your risk for coronary artery disease and to diagnose it.
To find out your risk for coronary artery disease
Your doctor will check your blood pressure and cholesterol levels and ask about other risk factors, such as your age and whether you smoke, to help find out your risk for getting heart disease.
To help find your risk, your doctor may do other tests. These include an ankle-brachial index test, C-reactive protein (CRP) test, or a coronary calcium scan.
If your doctor recommends a test, ask what it is for and why you need it. You can help decide if a test is right for you. Talk with your doctor to make that decision. See the topic Heart Tests: When Do You Need Them?
To diagnose coronary artery disease
If your doctor thinks you may have heart disease, you will need some tests to make sure. Most often, the first tests include:
- An electrocardiogram (EKG or ECG).
- A chest X-ray.
- Blood tests.
- An exercise electrocardiogram. This is also called a "stress test."
Other tests may include:
Treatment Overview
Treatment focuses on lowering your risk for heart attack and stroke and managing your symptoms. Lifestyle changes, medicine, and procedures are used.
Lifestyle changes
Lifestyle changes are the first step for anyone with coronary artery disease. Healthy habits can slow or even stop the disease and improve the quality and length of your life. These habits include:
- Quitting smoking and avoiding secondhand smoke.
- Eating a heart-healthy diet.
- Getting regular exercise.
- Getting to and staying at a healthy weight.
- Keeping a healthy mental attitude.
A cardiac rehabilitation program can help you make these changes.
It's also important to manage any health problems you have. If you have high blood pressure, high cholesterol, or diabetes, be sure you're doing everything you can to keep these conditions under control.
To learn what you can do, see Living With Heart Disease.
|
One Man's Story:  Alan, 73 "I've had to work at keeping my weight under control, and that has really helped my cholesterol. When you have heart disease, you learn to eat better for the rest of your life. And if you don't, you're asking for trouble."-Alan Read more about Alan and the lessons he's learned about diet and exercise. |
Medicines
You will probably have to take several medicines that lower your risk of a heart attack. These include:
- Aspirin or other antiplatelets to help prevent blood clots.
- Medicines that help lower blood pressure and reduce the workload on your heart. Examples are ACE inhibitors and beta-blockers.
- A statin to help lower cholesterol.
To manage symptoms, you might take an angina medicine, such as nitroglycerin.
Procedures
If your angina symptoms get worse even though you are taking medicines, you may think about having a procedure to improve blood flow to your heart. These include angioplasty and bypass surgery.
- Heart Disease: Should I Have Angioplasty for Stable Angina?
- Heart Disease: Should I Have Bypass Surgery?
Palliative care
Palliative care is a kind of care for people who have a serious illness. It's different from care to cure your illness. Its goal is to improve your quality of life-not just in your body but also in your mind and spirit.
You can have this care along with treatment to cure your illness. You can also have it if treatment to cure your illness no longer seems like a good choice.
Palliative care providers will work to help control pain or side effects. They may help you decide what treatment you want or don't want. And they can help your loved ones understand how to support you.
If you're interested in palliative care, talk to your doctor.
For more information, see the topic Palliative Care.
End-of-life care
If your heart disease is advanced, it may shorten your life. So you need to decide what kind of care you want at the end of your life.
It can be hard to have talks with your doctor and family about the end of your life. But making these decisions now may bring you and your family peace of mind. Your family won't have to wonder what you want. And you can spend your time focusing on your relationships.
You will need to decide if you want life-support measures if your health gets very bad. An advance directive is a legal document that tells doctors how to care for you at the end of your life. You also can say where you want to have care. And you can name someone who can make sure your wishes are followed.
For more information, see the topic Care at the End of Life.
Prevention
You can help prevent coronary artery disease by taking steps toward a heart-healthy lifestyle. A heart-healthy lifestyle can also help you reduce risk factors such as high cholesterol and high blood pressure.
Use lifestyle changes
- Quit smoking. Avoid secondhand smoke too. Quitting smoking may be the best thing you can do to prevent heart disease.
- Exercise. There are lots of ways that exercise boosts your heart health. It can improve cholesterol and blood pressure. It can also help you reach a healthy weight. Talk to your doctor before starting an exercise program to make sure that it's safe for you.
- Eat a heart-healthy diet. The way you eat can help you control your cholesterol and blood pressure.
- Stay at a healthy weight. Being active and eating healthy foods can help you stay at a healthy weight or lose weight if you need to.
Manage other health problems
Manage other health problems that raise your risk for a heart attack. These include diabetes, high blood pressure, and high cholesterol. A heart-healthy lifestyle can help you manage these problems. But you may also need to take medicine.
Reduce stress
Stress can hurt your heart. Keep stress low by talking about your problems and feelings, rather than keeping your feelings hidden. Try different ways to reduce stress, such as exercise, deep breathing, meditation, or yoga.
Deciding whether to take aspirin
Talk to your doctor before you start taking aspirin every day. Aspirin can help certain people lower their risk of a heart attack or stroke. But taking aspirin isn't right for everyone, because it can cause serious bleeding.
You and your doctor can decide if aspirin is a good choice for you based on your risk of a heart attack and stroke and your risk of serious bleeding. If you have a low risk of a heart attack and stroke, the benefits of aspirin probably won't outweigh the risk of bleeding.
What Happens
Coronary artery disease most often begins when the inside walls of the coronary arteries are damaged because of another health problem, such as high cholesterol, high blood pressure, diabetes, or smoking. This damage can lead to atherosclerosis, or hardening of the arteries. This means that plaque, made of fats and other substances, builds up in the coronary arteries.
If your heart disease gets worse, your arteries will narrow, and less blood will flow to your heart. You may start to have angina symptoms, such as chest pain or discomfort when you exercise or feel stressed. This is called stable angina.
In some cases, sudden and serious problems can happen. Some types of plaque are unstable. They can suddenly tear and cause blood clots to form. These clots block blood flow to your heart, causing a heart attack or unstable angina.
Complications of heart disease
Over time, you may have other health problems caused by coronary artery disease. Low blood flow can make it harder for your heart to pump. This can lead to heart failure or atrial fibrillation. Atrial fibrillation increases the risk of stroke.
Living With Heart Disease
A diagnosis of coronary artery disease can be hard to accept and understand. If you don't have symptoms, it may be especially hard to recognize that heart disease is serious and can lead to other health problems.
It's important to talk with your doctor to learn about the disease and what you can do to help manage it and keep it from getting worse.
Lifestyle changes
- Quit smoking, and avoid secondhand smoke. Quitting smoking is the best thing you can do to reduce your risk of future problems. When you quit, you quickly lower your risk of a heart attack.
- Exercise. Start an exercise program (if your doctor says it's safe). Try walking, swimming, biking, or jogging for at least 30 minutes on most, if not all, days of the week. Any activity you enjoy will work, as long as it gets your heart rate up.
- Eat a heart-healthy diet. This can help you keep your disease from getting worse. A chart (What is a PDF document?) that compares heart-healthy diets can help you see what foods are suggested in each plan. Heart-healthy foods include fruits, vegetables, high-fiber foods, fish, and foods low in sodium, saturated fat, and trans fat.
- Stay at a healthy weight. Being active and eating healthy foods can help you stay at a healthy weight or lose weight if you need to.
Your doctor may suggest that you attend a cardiac rehabilitation (rehab) program. In cardiac rehab, you will get education and support that help you build new, healthy habits, such as eating right and getting more exercise.
Medicines
Medicines are an important part of your treatment.
- Take your medicines exactly as directed. Do not stop taking your medicine unless your doctor tells you to.
- Control angina (including chest pain or discomfort) by taking medicines as prescribed and nitroglycerin when needed. To learn more, see the topic Quick Tips: Taking Charge of Your Angina.
- Get a flu vaccine every year.
Get help for depression
Depression and heart disease are linked. People with heart disease are more likely to get depressed. And if a person has both depression and heart disease, he or she may not stay as healthy as possible. This can make depression and heart disease worse.
If you think you may have depression, talk to your doctor. Take this short quiz to check your symptoms: Interactive Tool: Are You Depressed? For more information, see the topic Depression.
Manage other health problems
To reduce your risk of heart attack or stroke, you will need to control other health problems you may have. These problems include diabetes, high cholesterol, and high blood pressure.
Other steps to stay healthy
- Find emotional support. Think about joining a heart disease support group. Ask your doctor about the types of support that are available where you live. Meeting other people with the same problems can help you know you're not alone. Your family and friends can also give you support.
- Drink alcohol in moderation, if you drink. This means having 1 drink a day for women or 2 drinks a day for men.
- Manage stress and anger. Stress and anger can also hurt your heart. They might make your symptoms worse. Try different ways to reduce stress, such as exercise, deep breathing, meditation, or yoga.
- Seek help for sleep problems. Sleep apnea is a common problem in people who have heart disease.
- Have sex when you're ready. If you are worried about sex and your heart, talk with your doctor. Your doctor can help you know if your heart is healthy enough for sex.
Medications
Medicines are an important part of your treatment. Using them correctly can lower your risk of having a heart attack or dying from coronary artery disease.
Medicine to lower blood pressure and the heart's workload
- Angiotensin-converting enzyme (ACE) inhibitors
- Angiotensin II receptor blockers (ARBs)
- Beta-blockers
- Calcium channel blockers
- Diuretics
Medicine to prevent blood clots from forming and causing a heart attack
Aspirin, ibuprofen, and naproxen are all nonsteroidal anti-inflammatory drugs (NSAIDs) and can relieve pain and inflammation. But only aspirin will reduce your risk for heart attack or stroke. Don't substitute ibuprofen or naproxen for aspirin. If you need to take an NSAID for a long time, talk with your doctor to see if it is safe for you.
Medicine to lower cholesterol
Other cholesterol medicines may be used along with or instead of statins.
Medicine to manage angina symptoms
Stable angina can often be controlled with medicine such as:
- Nitrates (nitroglycerin and long-acting nitrates).
- Beta-blockers.
- Calcium channel blockers.
- Ranolazine (Ranexa).
If you take nitrates
Do not use erection-enhancing medicines such as sildenafil (Viagra), tadalafil (Cialis), or vardenafil (Levitra) if you take nitroglycerin or other nitrates for angina. Combined, these two drugs can cause a serious drop in blood pressure. Talk to your doctor. There are other medicines that may work instead to ease your angina.
For more help with controlling angina, see:
Help taking your medicines
Medicine is a powerful tool to help you manage your heart disease. To get the most of your medicines, take them as prescribed. This may be hard because of how many you have to take and their cost. You may also worry about side effects.
- Taking Medicines as Prescribed
- Dealing With Medicine Side Effects and Interactions
- Reducing Medicine Costs
You may have regular blood tests to monitor how the medicine is working in your body. Your doctor will likely let you know when you need to have the tests.
Surgery
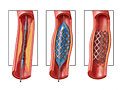
Sometimes coronary artery bypass graft surgery is needed to improve blood flow to the heart. During this surgery, a doctor connects (grafts) a healthy artery or vein from another part of your body to the narrowed or blocked coronary artery. The grafted artery goes around (bypasses) the narrowed or blocked part of the artery. The bypass provides a new pathway for blood to your heart.
If you have surgery, you'll still need to make changes in the way you eat and how much you exercise. These changes, along with not smoking, will give you the best chance of living a longer, healthier life. A cardiac rehabilitation program can help you make these healthy changes.
Angioplasty
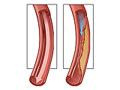
Angioplasty is a procedure that widens the coronary artery to improve blood flow to the heart. It is done using a thin, soft tube called a catheter, which is inserted in your artery.
Angioplasty is not surgery. It doesn't use large cuts (incisions) or require anesthesia to make you sleep.
Most of the time, stents are placed during angioplasty. The stent keeps the artery open. When stents are used, there is a smaller chance that the artery will become narrow again.
If you decide to have angioplasty, you'll still need to make changes in the way you eat and how much you exercise. These changes, along with not smoking, will give you the best chance of living a longer, healthier life. A cardiac rehabilitation program can help you make these healthy changes.
Other Places To Get Help
Organizations
Related Information
References
Other Works Consulted
- Budoff M, et al. (2006). Assessment of coronary artery disease by cardiac computed tomography: A scientific statement from the American Heart Association Committee on Cardiovascular Imaging and Intervention, Council on Cardiovascular Radiology and Intervention, and Committee on Cardiac Imaging, Council on Clinical Cardiology. Circulation, 114(16): 1761-1791.
- Chou R, et al. (2011). Screening asymptomatic adults with resting or exercise electrocardiography: A review of the evidence for the U.S. Preventive Services Task Force. Annals of Internal Medicine, 155(6): 375-385.
- Eckel RH, et al. (2013). 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. http://circ.ahajournals.org/content/early/2013/11/11/01.cir.0000437740.48606.d1.citation. Accessed December 5, 2013.
- Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents (2011). Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: Summary report. Pediatrics, 128(Suppl 5): S213-S256.
- Fihn SD, et al. (2012). ACCF/AHA/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation, 126(25): e354-e471.
- Fihn SD, et al. (2014). 2014 ACC/AHA/AATS/PCNA/SCAI/STS focused update of the guideline for the diagnosis and management of patients with stable ischemic heart disease. Circulation. DOI: 10.1161/CIR.0000000000000095. Accessed October 13, 2014.
- Fleg JL, et al. (2013). Secondary prevention of atherosclerotic cardiovascular disease in older adults: A scientific statement from the American Heart Association. Circulation, published online October 28, 2013. DOI: 10.1161/01.cir.0000436752.99896.22. Accessed November 22, 2013.
- Goff DC Jr, et al. (2013). 2013 ACC/AHA guideline on the assessment of cardiovascular risk: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation, published online November 12, 2013. DOI: 10.1161/01.cir.0000437741.48606.98. Accessed November 22, 2013.
- Hillis LD, et al. 2011 ACCF/AHA Guideline for coronary artery bypass graft surgery: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation, 124(23): e652-e735.
- Levine GN, et al. (2011). 2011 ACC/AHA/SCAI Guideline for percutaneous coronary intervention: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation, 124(23): e574-e651.
- O'Gara PT, et al. (2013). 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: Executive summary. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation, 127(4): e362-e425.
- Smith SC, et al. (2011). AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: A guideline from the American Heart Association and American College of Cardiology Foundation. Circulation, 124(22): 2458-2473. Also available online: http://circ.ahajournals.org/content/124/22/2458.full.
- Stone NJ, et al. (2013). 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation, published online November 12, 2013. DOI: 10.1161/01.cir.0000437738.63853.7a. Accessed November 18, 2013.
- Taylor AJ, et al. (2010). ACCF/SCCT/ACR/AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 - Appropriate use criteria for cardiac computed tomography: A Report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the Society of Cardiovascular Computed Tomography, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the American Society of Nuclear Cardiology, the North American Society for Cardiovascular Imaging, the Society for Cardiovascular Angiography and Interventions, and the Society for Cardiovascular Magnetic Resonance. Journal of the American College of Cardiology, 56(22): 1864-1894.
- U.S. Preventive Services Task Force (2009). Using nontraditional risk factors in coronary heart disease risk assessment. Available online: http://www.uspreventiveservicestaskforce.org/uspstf/uspscoronaryhd.htm.
- U.S. Preventive Services Task Force (2012). Screening for coronary heart disease with electrocardiography: Recommendation statement. Available online: http://www.uspreventiveservicestaskforce.org/uspstf/uspsacad.htm.
- Whelton PK, et al. (2017). 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults. Journal of the American College of Cardiology, published online November 13, 2017. DOI: 10.1016/j.jacc.2017.11.006. Accessed November 20, 2017.
Credits
ByHealthwise Staff
Primary Medical Reviewer Kathleen Romito, MD - Family Medicine
Martin J. Gabica, MD - Family Medicine
Adam Husney, MD - Family Medicine
Specialist Medical Reviewer Stephen Fort, MD, MRCP, FRCPC - Interventional Cardiology
Current as ofDecember 19, 2017
- Top of Page
Next Section:
Health Tools
Previous Section:
Topic Overview- Top of Page
Next Section:
Frequently Asked Questions
Previous Section:
Health Tools- Top of Page
Next Section:
Cause
Previous Section:
Frequently Asked Questions- Top of Page
Next Section:
Symptoms
Previous Section:
Cause- Top of Page
Next Section:
What Increases Your Risk
Previous Section:
Symptoms- Top of Page
Next Section:
When to Call a Doctor
Previous Section:
What Increases Your Risk- Top of Page
Next Section:
Exams and Tests
Previous Section:
When to Call a Doctor- Top of Page
Next Section:
Treatment Overview
Previous Section:
Exams and Tests- Top of Page
Next Section:
Prevention
Previous Section:
Treatment Overview- Top of Page
Next Section:
What Happens
Previous Section:
Prevention- Top of Page
Next Section:
Living With Heart Disease
Previous Section:
What Happens- Top of Page
Next Section:
Medications
Previous Section:
Living With Heart Disease- Top of Page
Next Section:
Surgery
Previous Section:
Medications- Top of Page
Next Section:
Angioplasty
Previous Section:
Surgery- Top of Page
Next Section:
Other Places To Get Help
Previous Section:
Angioplasty- Top of Page
Next Section:
Related Information
Previous Section:
Other Places To Get Help- Top of Page
Next Section:
References
Previous Section:
Related Information- Top of Page
Next Section:
Credits
Previous Section:
References- Top of Page
Current as of: December 19, 2017