Obesity
Topic Overview
What is obesity?
Obesity means you have an amount of body fat that may harm your health. Having too much body fat can lead to type 2 diabetes, heart disease, high blood pressure, arthritis, sleep apnea, and stroke.
Because of these risks, it is important to lose weight even if you don't feel bad now. It is hard to change eating habits and exercise habits. But you can do it if you make a plan.
How do you know if you are obese?
You can use a measurement called a body mass index, or BMI, along with your waist size, to decide whether your weight is dangerous to your health. The BMI is a combination of your height and weight. If you have a BMI of 30 or higher, unhealthy eating patterns, and too little physical activity, your extra weight is putting your health in danger.
Use the Interactive Tool: Is Your BMI Increasing Your Health Risks? to find out your body mass index.
Use the Interactive Tool: What Is Your Child's BMI? to check BMI in children ages 2 to 19.
People who carry too much fat around the middle, rather than around the hips, are more likely to have health problems. In women, a waist size of 35 in. (88 cm) or more raises the chance for disease. In men, a waist size of 40 in. (101 cm) or more raises the chance for disease.footnote 1
If you are Asian, your health may be at risk if you have a BMI of 27.5 or higher and you have unhealthy eating patterns and too little physical activity. Also, health problems are seen with a smaller waist size. In Asian women, a waist size of 32 in. (80 cm) or more raises the chance for disease. In Asian men, a waist size of 36 in. (90 cm) or more raises the chance for disease.footnote 2
Check this table to find your risk for disease using your body mass index and waist size.
What causes obesity?
When you take in more calories than you burn off, you gain weight. How you eat, how active you are, and other things affect how your body uses calories and whether you gain weight.
If your family members are obese, you may have inherited a tendency to gain weight. And your family also helps form your eating and lifestyle habits, which can lead to obesity.
Also, our busy lives make it harder to plan and cook healthy meals. For many of us, it's easier to reach for prepared foods, go out to eat, or go to the drive-through. But these foods are often high in saturated fat and calories. Portions are often too large. Work schedules, long commutes, and other commitments also cut into the time we have for physical activity.
You've tried diets, but you always gain the weight back. What can you do?
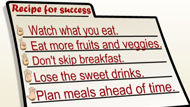
Focus on health, not diets. Diets are hard to stay on and usually don't work in the long run. It is very hard to stay with a diet that includes lots of big changes in your eating habits.
Instead of a diet, focus on lifestyle changes that will improve your health and achieve the right balance of energy and calories. To lose weight, you need to burn more calories than you take in. You can do it by eating healthy foods in reasonable amounts and becoming more active. And you need to do it every day.
Little steps mean a lot. Losing just 10% of your body weight can make a difference in your health.
Make a plan for change. Work with your doctor to create a plan that will work for you. Ask family members and friends for help in keeping with your plan. Ask your doctor to recommend a dietitian to help you with meal planning.
When you stray from your plan, don't get upset. Figure out what got you off track and how you can fix it.
How can you stay on your plan for change?
It's hard to change habits. You have to be ready. Make sure this is the right time for you. Are you ready to make a plan and stay on it? Do you have the support of your family and friends? Do you know what your first steps will be? Becoming healthier and staying that way is a lifelong effort.
Most people have more success when they make small changes, one step at a time. For example, you might eat an extra piece of fruit, walk 10 minutes more, or add more vegetables to your meals.
Studies show that people who keep track of what they eat are better at losing weight. Keep a notebook where you can write down everything you eat and drink each day. You may be surprised to see how much you are eating. Use a calorie counter to add up your calories. (You can find calorie counters online and at bookstores.)
As you keep track of calories, look at whether you skip meals, when you eat, how often you eat out, and how many fruits and vegetables you eat. Keep track of when you eat beyond feeling full and if you eat for reasons other than being hungry. This will help you see patterns that you may want to change.
You may want to write down the amount of physical activity you've had each day and compare the calories you burned to those you took in. Use the Interactive Tool: How Many Calories Did You Burn? to see how many calories you burn through daily activities.
Can you take medicines or have surgery to lose weight?
Surgery and medicines don't work by themselves. Most people also need to make changes in what they eat and how active they are.
Before your doctor will prescribe medicines or surgery, he or she will probably want you to work on healthier eating and activity for at least 6 months. Even if your doctor gives you medicines or recommends surgery, you will need to keep your new healthy habits for the rest of your life.
Frequently Asked Questions
Learning about obesity: | |
Being diagnosed: | |
Getting treatment: | |
Ongoing concerns: | |
Living with obesity: |
Health Tools
Health Tools help you make wise health decisions or take action to improve your health.
Cause
Obesity is a complex disease for which no single cause or cure exists. You gain weight when you take in more calories than you burn off. But obesity is influenced by many other things, including:
- Your habits. Eating unhealthy foods and overeating are easy in our culture today. Many things influence eating behavior, including emotions, habits, and the availability of food.
- Your lifestyle. Modern conveniences-such as elevators, cars, and the remote control for the television-cut activity out of our lives.
- Your genes. If one of your parents is obese, you are more likely to be obese than someone who has parents of healthy weight.
- Your friends and family. If they eat a lot of snack foods high in saturated fat, eat at irregular times, and skip meals, you probably will too. And if they are not physically active, you may not be either.
Other things influence your weight and whether you are physically active, including:
- Low self-esteem. Being overweight or obese may lower your self-esteem and lead to eating as a way to comfort yourself. Repeated failure at dieting also can affect your self-esteem and make it even harder to lose weight.
- Emotional concerns. Emotional stress, anxiety, or illnesses such as depression or chronic pain can lead to overeating. Some people eat to calm themselves, to avoid dealing with unpleasant tasks or situations, or to dampen negative emotions.
- Trauma. Distressing events-such as childhood sexual, physical, or emotional abuse; loss of a parent during childhood; or marital or family problems-can contribute to overeating.
- Alcohol. Alcohol (beer, wine, and mixed drinks) is very high in calories.
- Medicines or medical conditions. Some medical conditions and medicines may also cause weight gain. Examples include having Cushing's syndrome or hypothyroidism or taking certain antidepressants or corticosteroids.
Health Risks of Obesity
How obesity affects your health depends on many things, including your age, gender, where you carry your body fat, and how physically active you are.
Risk for diseases
If you are obese and have unhealthy eating or activity habits, you have a higher risk for gallstones, type 2 diabetes, high blood pressure, high cholesterol and triglycerides, coronary artery disease (CAD), a stroke, and sleep apnea, among other conditions.
Children who are obese are at risk for many of the same long-term health problems.
If you have healthier habits or lose weight, your risk for these conditions is reduced.
Where you carry fat
If fat builds up mostly around your stomach (sometimes called apple-shaped), you are at greater risk for type 2 diabetes, high blood pressure, high cholesterol, and coronary artery disease than people who are lean or people with fat around the hips (sometimes called pear-shaped). Your waist size affects your risk of health problems.
Health Benefits of Weight Loss
Research shows the following health benefits for weight loss:
- Weight loss may improve survival in those who have an obesity-related disease, especially type 2 diabetes.
- Blood pressure decreases with weight loss.
- People with type 2 diabetes who lost weight had lower blood sugar levels and were able to use less medicine to lower their blood sugar levels.
- Weight loss makes it easier for you to breathe.
Exams and Tests
Along with a regular medical checkup, you may have some tests to check on your health.
Your doctor may want to do blood tests to check for type 2 diabetes, thyroid or liver problems, and high cholesterol or high triglyceride levels.
Your doctor will check your blood pressure, ask about any medicines you are taking, and discuss your medical history and your family's medical history. He or she will ask how active you are, whether you drink alcohol (and how much), your history of weight gain, and how often you have tried to lose weight.
Knowing your waist size along with your body mass index (BMI) can help your doctor check your risk for type 2 diabetes and coronary artery disease (CAD).
Tests are available to estimate your body fat percentage (to find out about how much of your weight is fat). This is different from your BMI. With some of these tests, you may also learn your basal metabolic rate (BMR). Knowing your BMR can help your doctor or registered dietitian plan how many calories you need each day.
Early detection
Doctors use BMI to help screen for unhealthy weight. If you have a BMI of 30 or higher, your extra weight-as well as unhealthy eating patterns and too little physical activity-may be putting your health in danger. If you are Asian, your health may be at risk with a BMI of 27.5 or higher.footnote 2
Use the Interactive Tool: Is Your BMI Increasing Your Health Risks? to find your BMI.
If you're concerned about your child's weight
If you have concerns that your child is overweight or at risk of becoming so, ask your doctor to review your child's growth charts and medical history with you. If your child's BMI and growth pattern suggest a weight problem, your doctor will give your child an exam to look for problems that can cause weight gain. He or she may ask questions about eating and exercise habits. Regular checkups will also be important over time.
Use the Interactive Tool: What Is Your Child's BMI? to find out the BMI of your child age 2 or older.
Treatment Overview
Treatment for obesity will be most successful if you create a long-term plan with your doctor. A reasonable goal might be to begin making lifestyle changes by increasing physical activity and eating healthy foods. Your initial goal should be to improve your health, not to achieve an ideal weight.
Guidelines suggest a goal of losing 10% of your body weight in 6 months.footnote 1 Doctors often recommend that people make lifestyle changes for at least 6 months before trying medicines or surgery.
Your doctor may also suggest counseling. If you use food to cope with depression, loneliness, anxiety, or boredom, you need to learn new skills to deal with those feelings.
Eat less
Eating fewer calories while increasing activity is the best way to lose weight. Focus on smaller portion sizes.
See ChooseMyPlate for the amount of food you should eat.
People often convince themselves that they don't overeat. Keeping a food journal (What is a PDF document?) can help you find out how many calories you consume in a day. Then you can set a goal with your doctor or dietitian according to your needs.
Limiting your calories to very low levels might seem like the way to quick weight loss. But it can have serious negative effects on your body and your ability to keep the weight off.
Limiting calories and portion size-not limiting the types of foods you eat-causes more weight loss over the long term. For example, cutting only carbohydrate or fat will not cause any more weight loss than a healthful eating plan.
Eat healthier foods-don't diet
Rather than focusing on a particular type of diet, try to eat healthier foods. Don't try to restrict the foods you love. Eat less of them. Eat smaller portions.
Take a look at the dietary guidelines for good health.
A dietitian can show you how to make healthy changes in your eating habits and help you recognize your hunger signals. For more information, see the Weight-Loss Strategies and Programs section of this topic.
Increase activity
Physical activity helps you burn more calories. Overall, experts recommend doing moderate or vigorous activity to get and stay healthy.
One of the best ways to increase your activity is by walking.
Keep track of your steps with a step counter phone app or pedometer. If you have a desk job, you may be surprised to see how little you move in a typical day. Start with a goal of increasing your steps by 2,000 steps a day and work up to 10,000 to 12,000.
To find out how many calories are burned during various activities, use the Interactive Tool: How Many Calories Did You Burn?
For more information on exercise and fitness, see the topic Fitness: Getting and Staying Active.
Get checkups
See your doctor after 6 months to check your progress. Some people stop losing weight around this time, because their bodies adjust to fewer calories and their motivation starts to slip.
At this point your doctor may want you to increase your activity and revisit the dietitian to make further changes to your eating habits. Your goals may switch from losing more weight to keeping the weight off. Staying active is very important.
If you have lost weight but gained it back, don't be discouraged. It is not uncommon to try several times before weight comes off and stays off. Talk to your doctor about starting again. It may be helpful to work with others who are trying to lose weight by following a structured program.
When to consider medicines or surgery
If you do not lose weight, continue to gain weight, or have lost weight several times only to regain it, or if your doctor is concerned about a related health problem, you might need to try medicines or surgery.
Weight-Loss Strategies and Programs
Most weight-loss programs can help you lose weight at first. But you will lose more and have more health benefits if you can keep with it for a longer time. You need to find the right balance of eating and physical activity that you can keep doing or a program that works with your lifestyle.
Are you ready to make changes?
Before you begin treatment, decide if you are ready to make the lifestyle changes needed to lose weight. Losing weight and keeping it off can be hard. Think about successes that you had before and how you were able to achieve them.
If you are ready to make a plan for healthier eating, your doctor may suggest losing 10% of your weight at a rate of 1 lb (0.45 kg) to 2 lb (0.9 kg) a week as your first target. It is better that you maintain a small amount of loss rather than lose a lot of weight fast and gain it back.
Tips to help with your weight-loss program
- Set realistic goals. Many people expect to lose much more weight than is realistic. Think about why you want to lose weight, and prepare for slip-ups.
- Find what works best for you. Finding a plan that includes daily menus and recipes may be best.
- Get family and friends involved to provide support. Talk to them about why you are changing your eating habits and physical activity and how important losing weight is to you.
- Identify obstacles to losing weight. Keep a food journal (What is a PDF document?). Look at it to try to find things that cause you to overeat, such as stress or depression.
- Replace unhealthy food temptations with healthier foods such as fruit and low-fat yogurt.
- Get enough physical activity for weight loss. To find out how many calories are burned during various activities, see the Interactive Tool: How Many Calories Did You Burn?
Tips to help change how you eat
- Plan your meals and snacks ahead of time. This helps you eat regular meals and a balanced, nutritious diet. See Meal Planning: Menu and Grocery List (What is a PDF document?).
- Find your sources of added calories, such as snacking, drinking alcohol, or having soft drinks. Then reduce your intake of them.
- Cut unhealthy fat from your diet.
- Use lean meats and meat alternatives.
- Make healthy fast-food, restaurant, and convenience-food choices to stay with your healthy eating when you eat out.
- Keep unhealthy food out of the house.
- Eat before you go grocery shopping.
Tips for staying with it
Research shows that people who keep track of what they eat and drink each day have more success at losing weight:
- Keep a food journal to record everything you eat and drink.
- Pay attention to portion sizes.
- Use a calorie counter to check calories. You can find a calorie counter at a bookstore or online (see www.supertracker.usda.gov/foodtracker.aspx).
Keep up with your physical activity.
Think ahead about situations that may be hard. Ask yourself if you are eating for reasons other than hunger:
- Have you noticed a change in your eating or weight since a change occurred in your lifestyle or stress level?
- Do you use food as a reward?
- Do you eat whatever is most available because you don't plan ahead?
Weight-loss programs
Many commercial weight-loss programs (such as Weight Watchers or Lifesteps) and self-help or support groups (such as Overeaters Anonymous) are available. The quality and effectiveness of programs vary widely, from reputable obesity clinics associated with hospitals to quick weight-loss schemes that may even harm your health with untested "miracle" products.
When considering a weight-loss program, ask questions about the staff's qualifications and whether counseling is offered. Be aware that the advertising strategies for weight-loss programs and products, such as using celebrities and "before and after" pictures, are usually unrealistic.
Medications
Most weight-loss medicines for obesity work by making you feel less hungry or making you feel full sooner. They are used together with healthy eating habits and exercise.
Medicine is generally used only for those who have a body mass index (BMI) of 30 or higher. But they sometimes are used for those with a BMI of 27 or higher who are at risk for high blood pressure, high cholesterol, coronary artery disease, type 2 diabetes, and sleep apnea.footnote 1
Medicine choices
- Bupropion/naltrexone (Contrave) is a prescription medicine. Contrave may reduce your appetite. It may help you avoid overeating.
- Liraglutide (Saxenda) is a prescription medicine that is given by a shot once a day. It may help you eat less.
- Lorcaserin (Belviq) is a prescription medicine that you take twice a day. It can help you eat less and feel satisfied with eating smaller amounts of food.
- Orlistat (Xenical) is a prescription medicine that prevents some of the fat calories you eat from being absorbed in your intestines. Prescription orlistat is the only weight-loss medicine that is approved for children. It is meant to be used only in children over the age of 12.
- Orlistat (Alli) is also available over the counter. Alli contains half of the medicine that is in Xenical. Over-the-counter orlistat is not meant for use by anyone under the age of 18.
- Phentermine/topiramate (Qsymia) is a prescription medicine that combines the drugs phentermine and topiramate. Taking it once a day can help you eat less.
What to think about
Medicine doesn't work for everyone. And medicine alone is not as effective as when it is combined with healthy eating habits or activity.
Nonprescription weight-loss products aren't recommended. Some have dangerous side effects, and others have no proven benefit.
Surgery
Surgery may be an option if you have a body mass index (BMI) of 40 or more. It may also be an option if you have a BMI of 35 and another health problem related to your weight.
Use the Interactive Tool: Is Your BMI Increasing Your Health Risks? to calculate your BMI.
Experts are still debating whether surgery for obesity is okay for children.
The goal of surgery is to cause significant weight loss. This should reduce obesity-related health problems, including type 2 diabetes and high blood pressure.
Surgery can help you lose weight in a couple of ways. Restrictive operations (such as adjustable gastric band ) reduce how much food you can eat by making the stomach smaller. Malabsorptive operations (such as Roux-en-Y gastric bypass) make it harder for your body to digest and absorb food.
It is important to remember that you may still be obese or overweight after the surgery. Also, surgery will require you to make extreme changes in how you eat, such as eating only a few ounces of food at a time because the surgery creates a much smaller stomach.
Surgery choices
- Adjustable Gastric Band
- Gastric Sleeve Surgery
- Roux-En-Y Gastric Bypass
- Biliopancreatic Diversion and Biliopancreatic Diversion with Duodenal Switch
Nutrition concerns
After surgery, you will need to learn new ways to eat. You'll need to eat very slowly and chew your food well. You will not be able to drink for 30 minutes before eating, during your meal, and for 30 minutes after eating. If you don't make these changes, you may vomit frequently and have pain. You may also develop nutrition problems.
Your doctor may recommend calcium, iron, and vitamin supplements.
What to think about
All surgeries have risks. Discuss your treatment options with your doctor to decide what is best for you.
Most people who have surgery to treat obesity begin to lose weight quickly. Weight loss usually continues for about 2 years.
Risks common to all surgeries for weight loss include an infection in the incision, a leak from the stomach into the abdominal cavity or where the intestine is connected (resulting in an infection called peritonitis), and a blood clot that blocks blood flow in the lung (pulmonary embolism). Some people develop anemia or osteoporosis.
It is important to compare the risks of being obese with the risks of surgery.
Other Places To Get Help
Organization
Related Information
References
Citations
- National Heart, Lung, and Blood Institute, National Institutes of Health (2000). The Practical Guide: Identification, Evaluation, and Treatment of Overweight and Obesity in Adults (NIH Publication No. 00-4084). Available online: http://www.nhlbi.nih.gov/guidelines/obesity/prctgd_c.pdf.
- Purnell JQ (2011). Obesity. In EG Nabel, ed., ACP Medicine, section 6, chap. 12. Hamilton, ON: BC Decker.
Other Works Consulted
- Longitudinal Assessment of Bariatric Surgery (LABS) Consortium (2009). Perioperative safety in the longitudinal assessment of bariatric surgery. New England Journal of Medicine, 361(5): 445-454.
- American Cancer Society (2010). Cancer Prevention and Early Detection: Facts and Figures 2010. Atlanta: American Cancer Society. Available online: http://ww2.cancer.org/downloads/STT/Cancer_Prev_and_Early_Dect_2010.pdf.
- American Diabetes Association (2007). Eating with type 2 diabetes. Clinical Diabetes, 25(3): 104.
- American Gastroenterological Association (2002, reapproved 2008). AGA technical review on obesity. Gastroenterology, 123(3): 882-932. [Erratum in Gastroenterology, 123(5): 1752.]
- American Institute for Cancer Research (revised 2007). The new American plate for breakfast. Available online: http://www.aicr.org/publications/brochures/new-american-plate/pub_new_amer_plate_br.html.
- American Society for Metabolic and Bariatric Surgery (2011). Updated position statement on sleeve gastrectomy as a bariatric procedure. Available online: http://asmbs.org/guidelines-statements.
- Barlow SE (2007). Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary report. Pediatrics, 120(Suppl 4): S164-S192.
- Brethauer SA, et al. (2009). Systematic review of sleeve gastrectomy as staging and primary bariatric procedure. Surgery for Obesity and Related Diseases, 5: 469-475.
- DeLaet D, Schauer D (2011). Obesity in adults, search date September 2010. BMJ Clinical Evidence. Available online: http://www.clinicalevidence.com.
- Flier JS, Maratos-Flier E (2015). Biology of obesity. In DL Kasper et al., eds., Harrison's Principles of Internal Medicine, 19th ed., vol. 2, CD Chap 415e. New York: McGraw-Hill Education.
- Heber D, et al. (2010). Endocrine and nutritional management of the post-bariatric surgery patient: An Endocrine Society clinical practice guideline. Journal of Clinical Endocrinology and Metabolism, 95(11): 4823-4843. Available online: http://www.endo-society.org/guidelines/final/upload/FINAL-Standalone-Post-Bariatric-Surgery-Guideline-Color.pdf.
- Klein S, et al. (2011). Obesity. In S Melmed et al., eds., Williams Textbook of Endocrinology, 12th ed., pp. 1605-1632. Philadelphia: Saunders.
- National Institute of Diabetes and Digestive and Kidney Diseases (2008). Choosing a safe and successful weight-loss program. Available online: http://www.win.niddk.nih.gov/publications/choosing.htm.
- Paul IM, et al. (2009). Opportunities for the primary prevention of obesity during infancy. Advances in Pediatrics, 56: 107-133.
- Pories WJ (2008). Bariatric surgery: Risks and rewards. Journal of Clinical Endocrinology and Metabolism, 93(11, Suppl 1): S89-S96. Available online: http://jcem.endojournals.org/cgi/reprint/93/11_Supplement_1/s89.pdf.
- Rao G (2010). Office-based strategies for the management of obesity. American Family Physician, 81(12): 1449-1455.
- Tyo BM, et al. (2011). Effects of body mass index and step rate on pedometer error in a free-living environment. Medicine and Science in Sports and Exercise, 43(2): 350-356.
- U.S. Department of Health and Human Services (2011). Bariatric Surgery for Severe Obesity (NIH Publication No. 08-4006). Available online: http://www.win.niddk.nih.gov/publications/gastric.htm.
- U.S. Preventive Services Task Force (2012). Screening for and Management of Obesity in Adults. Available online: http://www.uspreventiveservicestaskforce.org/uspstf11/obeseadult/obesers.htm.
- U.S. Preventive Services Task Force (2017). Screening for obesity in children and adolescents: US Preventive Services Task Force recommendation statement. JAMA, 317(23): 2417-2426. DOI: 10.1001/jama.2017.6803. Accessed November 6, 2017.
Credits
ByHealthwise Staff
Primary Medical Reviewer E. Gregory Thompson, MD - Internal Medicine
Kathleen Romito, MD - Family Medicine
Martin J. Gabica, MD - Family Medicine
Adam Husney, MD - Family Medicine
Specialist Medical Reviewer Rhonda O'Brien, MS, RD, CDE - Certified Diabetes Educator
Current as ofNovember 16, 2017
- Top of Page
Next Section:
Health Tools
Previous Section:
Topic Overview- Top of Page
Next Section:
Cause
Previous Section:
Health Tools- Top of Page
Next Section:
Health Risks of Obesity
Previous Section:
Cause- Top of Page
Next Section:
Health Benefits of Weight Loss
Previous Section:
Health Risks of Obesity- Top of Page
Next Section:
Exams and Tests
Previous Section:
Health Benefits of Weight Loss- Top of Page
Next Section:
Treatment Overview
Previous Section:
Exams and Tests- Top of Page
Next Section:
Weight-Loss Strategies and Programs
Previous Section:
Treatment Overview- Top of Page
Next Section:
Medications
Previous Section:
Weight-Loss Strategies and Programs- Top of Page
Next Section:
Surgery
Previous Section:
Medications- Top of Page
Next Section:
Other Places To Get Help
Previous Section:
Surgery- Top of Page
Next Section:
Related Information
Previous Section:
Other Places To Get Help- Top of Page
Next Section:
References
Previous Section:
Related Information- Top of Page
Next Section:
Credits
Previous Section:
References- Top of Page
Current as of: November 16, 2017