Low Back Pain
Topic Overview
Is this topic for you?
This topic provides a general overview of low back pain. If you have been diagnosed with a herniated disc or spinal stenosis, see the topic Herniated Disc or Lumbar Spinal Stenosis.
What is low back pain?
Low back pain can happen anywhere below the ribs and above the legs. It is possible to hurt your back when you lift, reach, or twist. In fact, almost everyone has low back pain at one time or another.
What causes low back pain?
Causes of low back pain include:
- Overuse, strain, or injury.
- Aging.
- Herniated disc.
- Arthritis.
- Compression fractures.
- Illness.
- A spine problem you were born with.
Often doctors don't know what causes low back pain.
What are the symptoms?
Depending on the cause, low back pain can cause a range of symptoms. The pain may be dull or sharp. It may be in one small area or over a broad area. You may have muscle spasms.
Low back pain can also cause leg symptoms, such as pain, numbness, or tingling, often extending below the knee.
A rare but serious problem called cauda equina syndrome can occur if the nerves at the end of the spinal cord are squeezed. Seek emergency treatment if you have weakness or numbness in both legs or you lose bladder or bowel control.
Most low back pain is short-term (acute) and will go away in a few weeks. It is more likely to become long-lasting (chronic) if you are depressed or under stress.
How is low back pain diagnosed?
Your doctor will ask questions about your past health, symptoms, and activities. He or she will also do a physical exam. Your answers and the exam can help rule out a serious cause for the pain. In most cases, doctors are able to recommend treatment after the first exam.
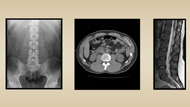
Tests such as X-rays, CT scans, and MRIs usually don't help.
But if you have a back pain problem that has lasted longer than 6 weeks, or if your doctor thinks you may have more than muscle pain, it might be time for one of these tests.
How is it treated?
Most low back pain will improve with basic first aid, which includes continuing to do light activity such as walking, and taking over-the-counter pain medicine as needed.
Walking is the simplest and maybe the best exercise for the lower back. It gets your blood moving and helps your muscles stay strong.
Your doctor or physical therapist can recommend more specific exercises to help your back muscles get stronger. These may include a series of simple exercises called core stabilization. Strengthening the muscles in your trunk can improve your posture, keep your body in better balance, and lower your chance of injury.
If your symptoms are severe or you still have symptoms after 2 weeks of self-care, see your doctor. You may need stronger pain medicines, or you might benefit from manual therapy.
Each of the various treatments for back pain work for some people but not for others. You may need to try different things to see which work best for you, such as:
- Spinal manipulation.
- Massage.
- Acupuncture.
Having ongoing (chronic) back pain can make you depressed. In turn, depression can have an effect on your level of pain and whether your back gets better. People with depression and chronic pain often benefit from both antidepressant medicines and counseling. Counseling can help you learn stress management and pain control skills.
How can you prevent low back pain from returning?
After you've had low back pain, you're likely to have it again. But there are some things you can do to help prevent it. And they can help you get better faster if you do have low back pain again.
To help keep your back healthy and avoid further pain:
- Practice good posture when you sit, stand, and walk. "Good posture" generally means your ears, shoulders, and hips are in a straight line.
- Get regular, low-impact exercise. Walk, swim, or ride a stationary bike. Stretch before you exercise.
- Sleep on your side.
- Watch your weight.
- Don't try to lift things that are too heavy for you. When you must lift, learn the right way to lift.
If you sit or stand for long periods at work:
- Sit or stand up straight, with your shoulders back.
- Make sure your chair fits you and has good back support.
- Take regular breaks to walk around.
If your work involves a lot of bending, reaching, or lifting:
- Talk to your human resources department to see if there are other ways you can do your work.
- Don't depend on a "back belt" to protect your back.
Frequently Asked Questions
Health Tools
Health Tools help you make wise health decisions or take action to improve your health.
- Anxiety: Stop Negative Thoughts
- Back Problems: Proper Lifting
- Depression: Stop Negative Thoughts
- Fitness: Increasing Core Stability
- Healthy Eating: Starting a Plan for Change
- Low Back Pain: Exercises to Reduce Pain
- Quitting Smoking: Getting Support
- Stop Negative Thoughts: Getting Started
- Stress Management: Breathing Exercises for Relaxation
- Stress Management: Doing Guided Imagery to Relax
- Stress Management: Doing Meditation
- Stress Management: Doing Progressive Muscle Relaxation
- Stress Management: Managing Your Time
- Stress Management: Practicing Yoga to Relax
- Stress Management: Relaxing Your Mind and Body
- Weight Management: Stop Negative Thoughts
Cause
Often doctors don't know what causes low back pain. The most common causes of low back pain are:
- Injury or overuse. This can include sprains or strains of soft tissues such as ligaments and muscles, fractures or compression fractures of bones, or injuries to the small joints between the bones of the spine.
- Pressure on nerve roots from conditions such as a herniated disc or spinal stenosis.
- Osteoarthritis, which is
usually caused by getting older.
- When osteoarthritis affects the small joints in the spine, it can lead to back pain by making the joints themselves stiff and sore and also by creating pressure on the nerve roots.
- Osteoarthritis in other joints, such as the hips, can cause you to limp or to change the way you walk. This can also lead to back pain.
Less common spinal conditions that can cause low back pain include:
- Ankylosing spondylitis, which is a form of arthritis that most often affects the spine.
- Bacterial infection in the bone, spinal discs, or spinal cord.
- Spinal tumors, which are growths on the bones and ligaments of the spine, on the spinal cord, or on nerve roots.
Symptoms
Symptoms of low back pain depend on the cause.
Back sprain or strain
Symptoms typically include:
- Muscle spasms, cramping, and stiffness.
- Pain in the back and sometimes in the buttock. It may come on quickly or gradually. It most often occurs in episodes. Certain movements make it worse, and doing light activities such as walking makes it feel better. The worst pain usually lasts 48 to 72 hours and may be followed by days or weeks of less severe pain.
Nerve-root pressure
Symptoms typically include:
- Leg pain. If pain extends below the knee, it is more likely to be due to pressure on a nerve than to a muscle problem. Most commonly, it's a pain that starts in the buttock and travels down the back of the leg as far as the ankle or foot. This pain pattern is known as sciatica (say "sy-AT-ih-kuh"). For more information, see the topic Sciatica.
- Nerve-related problems, such as tingling, numbness, or weakness in one leg or in the foot, lower leg, or both legs. Tingling may begin in the buttock and extend to the ankle or foot. Weakness or numbness in both legs, or loss of bladder and/or bowel control, are symptoms of cauda equina syndrome, which requires immediate medical attention.
Arthritis of the spine
Osteoarthritis of the spine usually causes pain that:
- Is worse in the back and hip region.
- Starts gradually, gets worse over time, and lasts longer than 3 to 6 months.
- Is generally worse in the morning or after prolonged periods of inactivity. Arthritis pain gets better when you move around.
Other conditions
Symptoms of diseases that affect the spine depend on the disease. They may include:
- Pain that is worse in the affected part of the spine (for instance, if there is a compression fracture, tumor, or infection).
- Pain that starts gradually, is constant, and may be sharp or a dull ache. Bed rest doesn't help and may make it worse (for example, tumors on the spine often cause night pain). The pain lasts longer than 2 to 3 weeks.
- Fever.
- Sensitivity of the spine to touch and pressure.
- Pain that wakes you up from sleep.
What Happens
The course of low back pain depends both on its cause and on how well you treat your back.
Most low back pain goes away within several weeks. But after you have had back pain once, you're more likely to have it again. Many people who recover have back pain again within a year, and most people will have it again sometime during their lives.
Long-lasting (chronic) pain not only makes you tired, irritable, and less productive and less active but also can trigger other problems. If your back pain causes you to use your body in different ways (for example, to limp or to sit differently), pain can develop in other areas of the body. Pain can also cause biochemical changes in your body that tend to keep the pain going.
What Increases Your Risk
A risk factor is something that increases your chances of having back pain. Having more risk factors means you have a higher chance of having back pain.
Physical and family risk factors
- Being middle-aged or older
- Being male
- Having a family history of back pain
- Having had a back injury before
- Being pregnant. A woman's back is significantly stressed by carrying a baby.
- Having had compression fractures of the spine
- Having had back surgery before
- Having spine problems since birth
Risk factors you can change with lifestyle changes
- Not getting regular exercise
- Doing a job or other activity that requires long periods of sitting, heavy lifting, bending or twisting, repetitive motions, or constant vibration, such as using a jackhammer or driving certain types of heavy equipment
- Smoking. People who smoke are more likely than people who don't smoke to have low back pain.
- Being overweight. Excess body weight, especially around the waist, may put strain on your back, although this has not been proved. But being overweight often also means being in poor physical condition, with weaker muscles and less flexibility. These can lead to low back pain.
- Having poor posture. Slumping or slouching on its own may not cause low back pain. But after the back has been strained or injured, bad posture can make pain worse. "Good posture" generally means your ears, shoulders, and hips are in a straight line. If this posture causes pain, you may have another condition such as a problem with a disc or bones in your back.
- Being under stress. Stress and other emotional factors are believed to play a major role in low back pain, particularly chronic low back pain. Many people unconsciously tighten their back muscles when they are under stress.
Risk factors you might change with medical treatment
- Having long periods of depression
- Using medicines long-term that weaken bones, such as corticosteroids
- Having an illness or disease that causes chronic coughing
When to Call a Doctor
Call 911 or other emergency services immediately if:
- Back pain occurs with chest pain or other symptoms of a heart attack.
- A person has signs of
damage to the spine after an injury (such as a car accident, fall, or direct
blow to the spine). Signs may include:
- Being unable to move part of the body.
- Severe back or neck pain.
- Weakness, tingling, or numbness in the arms or legs.
Call your doctor now if:
- You have new numbness in your legs or numbness in your legs that is getting worse.
- You have new weakness in your legs or weakness in your legs that is getting worse. (This could make it hard to stand up.)
- You have a new loss of bowel or bladder control.
- You have new or increased back pain with fever, painful urination, or other signs of a urinary tract infection.
- You have long-term back pain that suddenly gets much worse, and you did not cause it by being more active.
- You have a history of cancer or HIV infection, and you have new or increased back pain.
- Pain wakes you from sleep.
For more information, see the topic Back Problems and Injuries.
Watchful waiting
Most low back pain doesn't require a visit to a doctor.
If the pain doesn't get better after 1 or 2 days and you can't do your normal daily activities, call your doctor.
If you still have mild to moderate pain after at least 2 weeks of home treatment, talk with your doctor. He or she may want to check for problems that may be causing your back pain.
Who to see
The following health professionals can diagnose the cause of back pain, evaluate back injuries, and start treatment.
- Primary care providers:
You may also be referred to one of the following specialists:
- Physiatrist
- Neurosurgeon
- Rheumatologist
- Orthopedic surgeon
- Pain management specialist if low back pain has lasted for more than 3 months
- Cognitive-behavioral therapist
To prepare for your appointment, see the topic Making the Most of Your Appointment.
Exams and Tests
Your doctor will begin by asking questions about your medical history, your symptoms, and your work and physical activities. He or she will also do a physical exam. The questions and exam can help rule out a serious cause for your pain. Your doctor may also ask questions about stress at home and at work that may make you more susceptible to chronic pain.
If your back pain has lasted for less than 6 weeks, it may be best to wait to do any testing. This is because most back pain goes away on its own in a month or so.
But if you have a back pain problem that has lasted longer than 6 weeks, or if your doctor thinks you may have more than muscle pain, it might be time for a test.
Which tests are used?
Tests for low back pain include:
Sometimes other tests can be useful, such as a bone scan or an electromyogram and nerve conduction. These are used to look for bone, nerve, and muscle/nerve problems that might be causing low back pain.
Treatment Overview
Experts divide low back pain into two categories:
- Acute: This is pain that has lasted less than 3 months. Most people get better with home treatment.
- Chronic: This is pain that has lasted longer than 3 months. People with chronic back pain are usually helped with more intensive treatment.
Treatment for acute low back pain
Learn about the first aid steps you can take when you first get back pain, such as using heat or ice, taking medicine, and not resting too much.
Sometimes acute low back pain lasts longer than a few days, even after you try first aid steps. In such a case, you might add another treatment, such as acupuncture or manual therapy.
If your pain is very bad, your health care provider may recommend short-term use of a muscle relaxant. Some people consider epidural steroid shots.
 Answers From an Expert: "Stay as active as you can. Doctors used to say to rest, but it turns out that this is not the case. The more active you are, the better you will be, and the faster you will heal."-Dr. Robert Keller |
 One Woman's Story: "I thought, 'Okay, it will hurt for a day or two, and that's it.' But it lasted a lot longer. It took about 3 weeks. I guess we're used to fast cures. We take an aspirin, and the headache goes away. We take the antibiotic, and the infection disappears." -Lorna Read more about how Lorna learned to be patient with her back. |
Treatment for chronic low back pain
If you have chronic back pain, one type of treatment by itself doesn't always stop your pain. Spinal manipulation can work to relieve low back pain. Other treatments can too.
- Acupuncture
- Biofeedback
- Cognitive-behavioral therapy
- Comprehensive rehabilitation programs
- Massage
- Mindfulness-based stress reduction
If over-the-counter medicines combined with these treatments have not helped, your doctor may recommend another medicine. In some cases an antidepressant such as duloxetine can help. If pain is very bad, your doctor may have you try a week or two of an opioid pain reliever such as tramadol. Be sure to discuss the risks and the possible benefits of all medicines with your doctor.
Prevention
There is no clear evidence that you can prevent low back pain. But there are some things you can do that may help prevent it. And they can prepare you for faster recovery if you do have low back pain.
- Exercise to keep your back healthy and strong.
- Learn how to lift objects safely to protect your back.
- Think about your posture, whether you are sitting or standing.
- Try different sleeping positions that protect your back.
- Wear low-heeled shoes.
- Stay at a healthy weight to avoid excess strain on your lower back. For more information, see the topic Weight Management.
- If you smoke, quit.
- Eat a healthy diet.
- Manage stress.
To learn more, see Living With Low Back Pain.
Living With Low Back Pain
Almost everyone has low back pain at some time. The good news is that most low back pain will go away in a few days or weeks with some basic self-care. This includes first aid, self-massage and using heat or ice.
Basic self-care can also help prevent back problems from coming back.
 One Man's Story: "Some people get better fast, but others take a lot of time. That was my case. If you have back pain, do what you can for it, but don't be in a hurry. It usually gets better."-Jack Read more about how Jack learned that he didn't need surgery. |
Ease back into your daily activities
Some people are afraid that doing too much may make their pain worse. In the past, people stayed in bed, thinking this would help their backs. Now experts think that, in most cases, getting back to your normal activities is good for your back, as long as you avoid things that make your pain worse.
- For the first day or two of pain, take it easy. But as soon as possible, get back to your normal daily life and activities.
- Movement helps your muscles stay strong. Lying down for too long can make your problem worse.
- If you are an athlete, return to your activity carefully. Choose a low-impact option until your pain is under control.
- Getting Help Around the House
- Get Chores Done Without Making Your Pain Worse
- Low Back Pain and Sex
- Back to Work?
Avoid or change activities that cause pain
- Try to avoid bending, lifting, or reaching. These movements put extra stress on your back.
- When you sit, place a small pillow, a rolled-up towel, or a lumbar roll in the curve of your back for extra support.
- When you brush your teeth, put one foot on a stool.
- Don't wear shoes with high heels. Wear low-heeled shoes.
- Try different sleeping positions.
- If you sleep on your side, try putting a pillow between your knees.
- If you sleep on your back, use a pillow under your knees.
- You can also try rolling up a small towel and using it to support your lower back.
- Protect Your Back as You Lie Down
- Protecting Your Back While Sitting
- Moving From Sitting to Standing
- Posture: Standing and Walking
Pay attention to your body mechanics and posture
Body mechanics are the way you use your body. Posture is the way you sit or stand.
- To prevent a return of low back pain, you will need to take extra care when you lift. When you must lift, bend your knees and flex from your hips. Don't let your spine slump.
- Think about your posture, whether you are sitting or standing. Slumping or slouching alone may not cause low back pain. But after the back has been strained or injured, bad posture can make pain worse. "Good posture" generally means your ears, shoulders, and hips are in a straight line. If this posture causes pain, you may have another condition such as a problem with a disc or bones in your back.
Stretch and strengthen your back
When you no longer have acute pain, you may be ready for gentle strengthening exercises for your stomach, back, and legs, and perhaps for some stretching exercises. Exercise may not only help decrease low back pain but also may help you recover faster, prevent reinjury to your back, and reduce the risk of disability from back pain.
Walking is the simplest and perhaps the best exercise for the low back. Your doctor or a physical therapist can recommend more specific exercises to help your back muscles get stronger. These may include a series of simple exercises called core stabilization. The muscles of your trunk, or core, support your spine. Strengthening these muscles can improve your posture, keep your body in better balance, and decrease your chance of injury.
 One Man's Story: "I discovered that what you have to do is this: You do as much as you can."-Robert Read more about how Robert controls his back pain by staying active. |
Take care of stress
Stress and low back pain can create a vicious circle. You have back pain, and you begin to worry about it. This causes stress, and your back muscles begin to tense. Tense muscles make your back pain worse, and you worry more ... which makes your back worse ... and so on.
There are lots of ways to teach yourself to relax.
- Stress Management: Practicing Yoga to Relax
- Stress Management: Doing Guided Imagery to Relax
- Stress Management: Breathing Exercises for Relaxation
- Stress Management: Doing Progressive Muscle Relaxation
- Stress Management: Relaxing Your Mind and Body
- Stress Management: Managing Your Time
- Stress Management: Doing Meditation
 One Woman's Story: "I had too much to do and too little time. That means stress. And when I start stressing, my back starts aching. Before I knew it, my back was screaming at me."-Cathy Read more about how Cathy made time to deal with her stress. |
Manage your weight
Extra body weight, especially around the waist, may put strain on your back.
If you want to get to a healthy weight and stay there, lifestyle changes will work better than dieting.
Here are the three steps to reaching a healthy weight:
- Eat a
healthy diet.
- You may be tempted to do a diet overhaul and change everything about the way you eat. But you will be more successful at staying with the changes you make if you pick just one eating habit at a time to work on.
- Getting plenty of calcium and vitamin D may help prevent osteoporosis, which can lead to compression fractures and low back pain.
- Get moving. Try to make physical activity a regular part of your day, just like brushing your teeth. Start small, and build up over time. Moderate activity is safe for most people, but it's always a good idea to talk to your doctor before you start an exercise program.
- Change your thinking. Our thoughts have a lot to do with how we feel and what we do. If you can stop your brain from telling you discouraging things and have it start encouraging you instead, you may be surprised at how much healthier you'll be-in mind and body.
Quit smoking
People who smoke take longer to heal-from any injury, not just back pain. If you stop smoking, you may feel better sooner.
People who smoke are also much more likely to have back pain than people who don't smoke. This is because the nicotine and other toxins from smoking can keep spinal discs from getting all the nutrients they need from the blood, making disc injury more likely. These discs cushion the bones in your spine. An injured disc can cause low back pain.
Smoking also increases your risk of bone loss (osteoporosis).
Medications
Medicine can decrease low back pain and reduce muscle spasms in some people. But medicine alone isn't an effective treatment for low back pain. It should be used along with other treatments, such as walking and using heat or ice.
Medicine choices
There are several medicines your doctor may recommend, depending on how long you have had pain, what other symptoms you have, and your medical history. Be safe with medicines. Read and follow all instructions on the label.
The medicines recommended most often are:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen. These seem to be the most effective over-the-counter pain relievers for low back pain. But if you can't take NSAIDs, you can try acetaminophen. You can buy these medicines without a prescription. Some of them also come in stronger doses. For those, you'll need a prescription.
- Muscle relaxants. These medicines can help with severe muscle spasms that happen when the back pain starts (acute phase). Side effects, such as drowsiness, are common.
- Opioid pain relievers. These are very strong medicines that are sometimes tried to ease severe back pain that has not been controlled by other medicines. They are usually taken for only 1 to 2 weeks.
- Antidepressants. Some of these medicines, such as duloxetine, not only treat depression but also may help with chronic pain.
Other medicines sometimes used for low back pain are:
- Anesthetic or steroid injections. These have been prescribed for chronic low back pain, but they have not been researched enough to know if they work well for back pain. They may give short-term relief from leg pain related to a back problem.
- Botox injection. This is a shot into the back muscles. It has not been well tested for chronic low back pain.
Medicines that work for some people don't work for others. Let your doctor know if the medicine you are taking doesn't work for you. You may be able to take another medicine for your back pain.
Surgery
When you're in a lot of pain, you might wonder if you need surgery to fix what's wrong so that you can feel better.
Every case is different. But most people don't need surgery for low back pain.
When surgery may help
Most back surgeries are done to treat nerve pain from herniated discs. Surgery might be an option when a disc problem causes pain in your leg that prevents you from doing everyday tasks. You may have pain, numbness, or tingling through your buttock and down the back of your leg (sciatica) or in the front of your thigh.
Other problems that may require surgery include:
- A spinal fracture caused by an injury.
- An infection in your spine.
- A problem that causes your spine to be unstable.
- A tumor in your spine.
- Spinal stenosis.
- Loss of feeling or weakness in your back or legs that gets worse over time.
- Loss of control of your bowel or bladder.
Having surgery for a herniated disc or another back problem is a big decision. Talk to your doctor about it.
Surgery choices
There are several types of back surgery. Some, like a discectomy, can help people who have severe symptoms. Others have not been proved to work.
If you do need surgery, you and your doctor will decide which type is best for you. Types of surgeries include:
- Discectomy.
- Percutaneous discectomy.
- Laminectomy for spinal stenosis.
- Kyphoplasty and vertebroplasty.
- Surgeries for tumors and infection.
- Spinal fusion.
Rehabilitation after surgery
A comprehensive rehabilitation program is very important after most back surgery. As you regain flexibility, recondition your back and stomach muscles, and increase your endurance for activity, you increase your chances of treatment success.
If you are unable or unwilling to commit to physical therapy after surgery, you may not be a good candidate for surgery.
Deciding whether to have surgery
If you and your doctor are considering surgery, get as much information as you can about possible results, and consider whether you will be willing to do physical therapy after surgery. It is also a good idea to get a second opinion before you decide to have surgery.
- Interactive Tool: Should I Consider Surgery for My Low Back Problem?
- Herniated Disc: Should I Have Surgery?
Back surgery isn't always successful. Depending on the condition, you may still have back pain after surgery.
Other Treatment
You can choose from a number of treatments for your low back pain. Because some of these treatments are new or not yet well researched, they may not be covered by health insurance.
The following complementary treatments are often used for low back pain.
- Massage may reduce low back pain for a short time. It is probably most effective if you also learn to do exercises for your back and learn the best ways to lift and move to protect your back.
- Biofeedback hasn't been well studied as a treatment for low back pain. Recent research hasn't shown that biofeedback is effective for controlling low back pain.
- Acupuncture may help reduce pain and increase the ability to be active for a short time after treatment but not any more than other treatments.footnote 1
- Acupressure uses pressure on certain points in the body to decrease symptoms. Small studies suggest that acupressure reduces pain and allows a person to be more active.footnote 2
- Relaxation techniques can help reduce muscle tension, stress, and depression.
- Yoga is another way to stay active and get help with relaxation and managing stress. Small studies suggest that yoga classes may help people with chronic low back pain control their symptoms and stay more active.footnote 3, footnote 4 It is not clear whether yoga is more helpful than other activity or treatment for chronic low back pain. There are different types of yoga. Talk to your doctor before you start a yoga program.
- Capsaicin cream may help relieve pain.footnote 5 Capsaicin is a substance contained in cayenne peppers. Capsaicin cream is applied directly to the skin over the painful area.
Here are some other treatment choices to think about:
- Self-care techniques:
- Back school teaches you all about back care, how to stand and sit, and how to move your body in a safer way.
- A pain management clinic is a place where you can learn how to cope with chronic pain.
- Electric currents:
- Transcutaneous electrical nerve stimulation (TENS) gives brief pulses of electricity to nerve endings in the skin to relieve pain.
- Spinal cord stimulation uses an electrical current to treat chronic pain.
- Other
procedures:
- Intradiscal electrothermal therapy (IDET) gets rid of nerve fibers that have grown from the outer layers of the disc to the inside of the disc.
- Nerve blocks may numb certain nerves.
- Low-level laser therapy, which uses targeted light energy to decrease pain and promote healing.
Experimental treatments
New and experimental treatments are constantly being developed and offered to people who have low back pain. If you are considering such a treatment, be sure to ask your doctor for two things:
- The scientific evidence that shows that the treatment works and is safe.
- The results that your doctor has seen in his or her own practice.
Experimental treatments include:
- Surgery to replace a ruptured or herniated disc with an artificial disc. This treatment has been approved by the U.S. Food and Drug Administration (FDA). Long-term studies haven't been done.
- Botulinum toxin (Botox) injection. This may relax painful muscle spasms in the low back.
- Radiofrequency ablation of nerves. This may reduce chronic low back pain in some people by preventing pain signals from reaching the brain. It is sometimes used for pain from problems with the small joints in the spine called facet joints.
- An intrathecal pain pump. This is a small tube inserted under the skin and deeper tissues along the midline of the back and into the spinal canal. The tube connects to a small reservoir of medicine inserted under the skin of your belly. The medicine is regularly delivered to the area of pain through the tube.
Coping With Chronic Back Pain
Low back pain can take a toll on your mental health. You may feel fear, frustration, and anger or have depression and anxiety because of ongoing pain. Those common reactions can make your pain last even longer. If pain is starting to get you down:
- Let people know when you need a helping hand. Ask family members or friends to help out with physical tasks you can't do right now.
- Be honest with your doctor about your pain. Ask for a referral to a counselor or pain management specialist. A prescription antidepressant or antianxiety medicine may also help with chronic pain.
- Work with your health professionals and your work supervisor to make a return-to-work plan, if needed. Ask for an ergonomic consultation if you need to learn how to do some of your job duties differently to avoid hurting your back again.
 One Man's Story: "I started feeling sad and angry a lot. I didn't want to do anything. My back was hurting more. I was having trouble focusing on my work. My life just started feeling smaller and smaller."-Ravi Read more about how Ravi learned he had depression and how he fought back. |
Emotional support is important
You may have to lean on friends and family when facing difficult situations caused by chronic pain or other problems. Your loved ones can play an important role in supporting your recovery. Your doctor and community also may give you extra support.
Asking for support from others is not always easy. It can be hard to tell someone about your problems. But don't be afraid to ask for help.
Where you can get support
- Family. Family members can help you cope by giving you comfort and encouragement.
- Friends. Building strong relationships with others is important for your emotional well-being. Helping is a big part of friendship. At times you may be the one who encourages a friend.
- Counseling. Professional counseling can help you cope with situations that interfere with your life and cause stress. Counseling can help you understand and deal with your pain. You can learn ways to stop negative thoughts. See the topic Stop Negative Thoughts: Choosing a Healthier Way of Thinking.
- Your doctor. Find someone you trust and feel comfortable with. Be open and honest about your fears and concerns. Your doctor can help you get the right treatments, including treatment for depression or other problems.
- Religious groups. Religious or spiritual groups may help you meet people and get involved in the community. Some religious organizations can help you get counseling or other social support services.
- Social groups. Social groups can help you meet new people and get involved in activities you enjoy.
- Community support groups. In a support group, you can talk to others who have dealt with the same problems or illness as you. You can encourage one another and learn ways of coping with tough emotions.
 One Woman's Story: "I really work at finding the good things in my day. It helps me get through the day, and I think it makes my pain not bother me as much."-Patty Read more about how Patty used positive thinking to help her back pain. |
How friends and family can help
Your loved ones can offer support by:
- Giving encouragement. This can keep you from feeling hopeless or alone.
- Offering to help. Getting a helping hand can keep you from feeling overwhelmed. This may include helping with small daily tasks or bigger problems.
- Going to medical visits. Your loved ones can offer support by being involved in your medical care.
- Being honest and realistic. Make sure your loved ones understand how serious the problem is. They can help by not setting unreachable goals or by not acting like the problem will just go away.
- Respecting your wishes. You are responsible for your decisions. Your loved ones can offer support and encouragement without interfering with your major decisions.
Having trouble getting support from friends and family? There are steps you can take to make your social support stronger.
Staying active
Having chronic back pain can make exercising-even walking-difficult. Being active is often the last thing you want to think about.
But the truth is that easing back into daily activity and physical therapy exercises can help relieve back pain and can lead to long-term improvement for low back pain.footnote 6
So be as active as you can. Take short walks as often as you can. Talk to a physical therapist, chiropractor, osteopathic doctor, or physiatrist about exercises you can do.
Other Places To Get Help
Organizations
Related Information
References
Citations
- Furlan AD, et al. (2005). Acupuncture and dry-needling for low back pain. Cochrane Database of Systematic Reviews (1).
- Hsieh LL, et al. (2006). Treatment of low back pain by acupressure and physical therapy: Randomised controlled trial. BMJ, 333(7543): 696-700.
- Tilbrook HE, et al. (2011). Yoga for chronic low back pain: A randomized trial. Annals of Internal Medicine, 155(9): 569-578.
- Sherman KJ, et al. (2011). A randomized trial comparing yoga, stretching, and a self-care book for chronic low back pain. Archives of Internal Medicine, 171(22): 2019-2026.
- Gagnier JJ, et al. (2016). Herbal medicine for low back pain: A Cochrane review. Spine, 41(2): 116-133. DOI: 10.1097/BRS.0000000000001310. Accessed June 17, 2016.
- Chou R (2010). Low back pain (chronic), search date April 2009. Online version of BMJ Clinical Evidence: http://www.clinicalevidence.com.
Other Works Consulted
- Agency for Healthcare Research and Quality (2010). Complementary and Alternative Therapies for Back Pain II (Evidence Report/Technology Assessment No. 194). Rockville, MD: Agency for Healthcare Research and Quality. Also available online: http://www.ahrq.gov/downloads/pub/evidence/pdf/backpaincam/backcam2.pdf.
- Carragee EJ (2005). Persistent low back pain. New England Journal of Medicine, 352(18): 1891-1898.
- Carragee EJ, Hannibal M (2004). Diagnostic evaluation of low back pain. Orthopedic Clinics of North America, 35(2004): 7-16.
- Chaiamnuay S, et al. (2006). Risks versus benefits of cyclooxygenase-2-selective nonsteroidal antiinflammatory drugs. American Journal of Health-System Pharmacy, 63(19): 1837-1851.
- Chaparro LE, et al. (2014). Opioids compared with placebo or other treatments for chronic low back pain: an update of the Cochrane review. Spine, 39(7): 556-563. DOI: 10.1097/BRS.0000000000000249. Accessed February 6, 2015.
- Chou R, et al. (2009). Imaging strategies for low-back pain: Systematic review and meta-analysis. Lancet, 373(9662): 463-472.
- Chou R, et al. (2009). Interventional therapies, surgery and interdisciplinary rehabilitation for low back pain: An evidence-based clinical practice guideline from the American Pain Society. Spine, 34(10): 1066-1077.
- Chou R, et al. (2011). Diagnostic imaging for low back pain: Advice for high-value health care from the American College of Physicians. Annals of Internal Medicine, 154(3): 181-189.
- Chou R, et al. (2017). Nonpharmacologic therapies for low back pain: A systematic review for an American College of Physicians clinical practice guideline. Annals of Internal Medicine, 166(7): 493-505. DOI: 10.7326/M16-2459. Accessed April 19, 2017.
- Chou R, et al. (2017). Systemic pharmacologic therapies for low back pain: A systematic review for an American College of Physicians clinical practice guideline. Annals of Internal Medicine, 166(7): 480-492. DOI: 10.7326/M16-2458. Accessed April 19, 2017.
- Deyo RA, et al. (2004). Spinal-fusion surgery-The case for restraint. New England Journal of Medicine, 350(7): 722-726.
- Furlan AD, et al. (2015). Massage for low-back pain. Cochrane Database of Systematic Reviews (9). DOI: 10.1002/14651858.CD001929.pub3. Accessed October 30, 2015.
- Garra G, et al. (2010). Heat or cold packs for neck and back strain: A randomized controlled trial of efficacy. Academic Emergency Medicine, 17(5): 484-489.
- Kanayama M, et al. (2007). A minimum 10-year follow-up of posterior dynamic stabilization using Graf artificial ligament. Spine, 32(18): 1992-1996.
- Kovacs FM, et al. (2003). Effect of firmness of mattress on chronic non-specific low-back pain: Randomised, double-blind, controlled, multicentre trial. Lancet, 362(9396): 1599-1604.
- Mercier LR (2008). The back. In Practical Orthopedics, 6th ed., pp. 143-184. Philadelphia: Mosby Elsevier.
- Modic MT, et al. (2005). Acute low back pain and radiculopathy: MR Imaging findings and their prognostic role and effect on outcome. Radiology, 237(2): 599-604.
- Qaseem A, et al. (2017). Noninvasive treatments for acute, subacute, and chronic low back pain: A clinical practice guideline from the American College of Physicians. Annals of Internal Medicine, 166(7): 514-530. DOI: 10.7326/M16-2367. Accessed April 19, 2017.
- Roelofs PDDM, et al. (2008). Non-steroidal anti-inflammatory drugs for low back pain. Cochrane Database of Systematic Reviews (1).
- Shanthanna H, et al. (2017). Benefits and safety of gabapentinoids in chronic low back pain: A systematic review and meta-analysis of randomized controlled trials. PLOS Medicine, 14(8): e1002369. DOI: 10.1371/journal.pmed.1002369. Accessed November 6, 2017.
- Tay BKB, et al. (2014). Disorders, diseases, and injuries of the spine. In HB Skinner, PJ McMahon, eds., Current Diagnosis and Treatment in Orthopedics, 5th ed., pp. 156-229. New York: McGraw-Hill.
- Urquhart DM, et al. (2008). Antidepressants for non-specific low back pain. Cochrane Database of Systematic Reviews (1).
Credits
ByHealthwise Staff
Primary Medical Reviewer William H. Blahd, Jr., MD, FACEP - Emergency Medicine
Adam Husney, MD - Family Medicine
E. Gregory Thompson, MD - Internal Medicine
Specialist Medical Reviewer Kathleen Romito, MD - Family Medicine
Current as ofFebruary 23, 2018
- Top of Page
Next Section:
Health Tools
Previous Section:
Topic Overview- Top of Page
Next Section:
Cause
Previous Section:
Health Tools- Top of Page
Next Section:
Symptoms
Previous Section:
Cause- Top of Page
Next Section:
What Happens
Previous Section:
Symptoms- Top of Page
Next Section:
What Increases Your Risk
Previous Section:
What Happens- Top of Page
Next Section:
When to Call a Doctor
Previous Section:
What Increases Your Risk- Top of Page
Next Section:
Exams and Tests
Previous Section:
When to Call a Doctor- Top of Page
Next Section:
Treatment Overview
Previous Section:
Exams and Tests- Top of Page
Next Section:
Prevention
Previous Section:
Treatment Overview- Top of Page
Next Section:
Living With Low Back Pain
Previous Section:
Prevention- Top of Page
Next Section:
Medications
Previous Section:
Living With Low Back Pain- Top of Page
Next Section:
Surgery
Previous Section:
Medications- Top of Page
Next Section:
Other Treatment
Previous Section:
Surgery- Top of Page
Next Section:
Coping With Chronic Back Pain
Previous Section:
Other Treatment- Top of Page
Next Section:
Other Places To Get Help
Previous Section:
Coping With Chronic Back Pain- Top of Page
Next Section:
Related Information
Previous Section:
Other Places To Get Help- Top of Page
Next Section:
References
Previous Section:
Related Information- Top of Page
Next Section:
Credits
Previous Section:
References- Top of Page
Current as of: February 23, 2018