Top of the pageCheck Your Symptoms
Rash, Age 11 and Younger
Topic Overview
Healthy skin is a barrier between the inside of the body and the outside environment. A rash means some change has affected the skin. A rash is generally a minor problem or is part of an illness that will go away on its own. A rash may be caused by contact with a substance outside the body, such as poison ivy (contact dermatitis), or by other more serious illnesses, such as measles or scarlet fever (strep throat with rash).
Generalized rashes over the whole body that are caused by viruses are more common in babies and young children than in adults. A rash may be caused by a viral illness if the child also has a cold, a cough, or diarrhea, or is in a day care setting where he or she is with other children with viral illnesses. Most rashes caused by viruses are not serious and usually go away over a few days to a week. Home treatment is often all that is needed to treat these rashes.
After a child has had a rash caused by a virus, his or her body generally builds an immunity to that virus. This immunity protects the child from getting that specific viral illness and rash again. Common rashes caused by viruses include:
- Chickenpox (varicella). This rash is a common, contagious illness caused by a type of herpes virus.
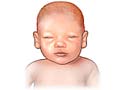
- Fifth disease. This facial rash looks like the cheeks have been slapped. It also causes a lacy, pink rash on the arms and legs, torso, and buttocks.
- Roseola (roseola infantum). This rash occurs about 3 days after a high fever.
- Unknown virus. Sometimes the specific virus that causes a rash is never known.
Localized rashes which affect one area of the body have many different causes and may go away with home treatment. Common localized rashes that occur during childhood include:
- Diaper rash. This rash is caused by rubbing, moisture, chemicals, or bacteria in the baby's urine or stool; substances in disposable diapers; or soaps used to wash cloth diapers.
- Impetigo. This bacterial skin infection is caused by strep or staph bacteria.
- Heat rash (prickly heat). This rash often results from a well-meaning parent dressing his or her baby too warmly, but it can happen to any baby in very hot weather.
- Cold sores. These are sometimes called fever blisters. Cold sores are clusters of small blisters on the lip and outer edge of the mouth caused by the herpes simplex virus.
- Contact dermatitis. This rash is caused by contact with a substance, such as food, soap, or lotion, that causes an allergic reaction. Most contact dermatitis is mild and goes away when your child's skin no longer comes in contact with the substance.
- Cradle cap. Cradle cap is an oily, yellow scaling or crusting on a baby's scalp. It is common in babies and is easily treated. Cradle cap is not a part of any illness and does not mean that a baby is not being well cared for.
Rashes that may require a visit to a doctor include:
- Lyme disease, which is caused by a bacteria carried by deer ticks in some areas. A characteristic expanding red rash usually occurs at the site of the tick bite and is followed by flu-like symptoms, such as a headache, chills, fever, body aches, and stiffness.
- A rash that looks like a sunburn and a fever of 102°F (38.9°C) or higher. This type of rash may be caused by a rare condition called toxic shock syndrome.
- A very rare and serious type of generalized red rash called toxic epidermal necrolysis (TEN). This type of rash may cause the skin to peel away, leaving large areas of tissue that weep or ooze fluid like a severe burn. TEN may occur after the use of some medicines.
To know how serious the rash is, other symptoms that occur with the rash must be evaluated. Check your child's symptoms to decide if and when your child should see a doctor.
Check Your Symptoms
Many things can affect how your body responds to a symptom and what kind of care you may need. These include:
- Your age. Babies and older adults tend to get sicker quicker.
- Your overall health. If you have a condition such as diabetes, HIV, cancer, or heart disease, you may need to pay closer attention to certain symptoms and seek care sooner.
- Medicines you take. Certain medicines, herbal remedies, and supplements can cause symptoms or make them worse.
- Recent health events, such as surgery or injury. These kinds of events can cause symptoms afterwards or make them more serious.
- Your health habits and lifestyle, such as eating and exercise habits, smoking, alcohol or drug use, sexual history, and travel.
Try Home Treatment
You have answered all the questions. Based on your answers, you may be able to take care of this problem at home.
- Try home treatment to relieve the symptoms.
- Call your doctor if symptoms get worse or you have any concerns (for example, if symptoms are not getting better as you would expect). You may need care sooner.
If you're not sure if a child's fever is high, moderate, or mild, think about these issues:
With a high fever:
- The child feels very hot.
- It is likely one of the highest fevers the child has ever had.
With a moderate fever:
- The child feels warm or hot.
- You are sure the child has a fever.
With a mild fever:
- The child may feel a little warm.
- You think the child might have a fever, but you're not sure.
Abnormal bleeding means any heavy or frequent bleeding or any bleeding that is not normal for you. Examples of abnormal bleeding include:
- Nosebleeds.
- Vaginal bleeding that is different (heavier, more frequent, at a different time of month) than what you are used to.
- Rectal bleeding and bloody stools.
- Bloody or pink urine.
- Gums that bleed easily when you eat or gently brush your teeth.
When you have abnormal bleeding in one area of your body, it's important to think about whether you have been bleeding anywhere else. This can be a symptom of a more serious health problem.
Certain health conditions and medicines weaken the immune system's ability to fight off infection and illness. Some examples in children are:
- Diseases such as diabetes, cystic fibrosis, sickle cell disease, and congenital heart disease.
- Steroid medicines, which are used to treat a variety of conditions.
- Medicines taken after organ transplant.
- Chemotherapy and radiation therapy for cancer.
- Not having a spleen.
Symptoms of infection may include:
- Increased pain, swelling, warmth, or redness in or around the area.
- Red streaks leading from the area.
- Pus draining from the area.
- A fever.
Temperature varies a little depending on how you measure it. For children up to 11 years old, here are the ranges for high, moderate, and mild according to how you took the temperature.
Oral (by mouth), ear, or rectal temperature
- High: 104°F (40°C) and higher
- Moderate: 100.4°F (38°C) to 103.9°F (39.9°C)
- Mild: 100.3°F (37.9°C) and lower
A forehead (temporal) scanner is usually 0.5°F (0.3°C) to 1°F (0.6°C) lower than an oral temperature.
Armpit (axillary) temperature
- High: 103°F (39.5°C) and higher
- Moderate: 99.4°F (37.4°C) to 102.9°F (39.4°C)
- Mild: 99.3°F (37.3°C) and lower
Note: For children under 5 years old, rectal temperatures are the most accurate.
Symptoms of serious illness in a baby may include the following:
- The baby is limp and floppy like a rag doll.
- The baby doesn't respond at all to being held, touched, or talked to.
- The baby is hard to wake up.
Symptoms of serious illness may include:
- A severe headache.
- A stiff neck.
- Mental changes, such as feeling confused or much less alert.
- Extreme fatigue (to the point where it's hard for you to function).
- Shaking chills.
Sudden tiny red or purple spots or sudden bruising may be early symptoms of a serious illness or bleeding problem. There are two types.
Petechiae (say "puh-TEE-kee-eye"):
- Are tiny, flat red or purple spots in the skin or the lining of the mouth.
- Do not turn white when you press on them.
- Range from the size of a pinpoint to the size of a small pea and do not itch or cause pain.
- May spread over a large area of the body within a few hours.
- Are different than tiny, flat red spots or birthmarks that are present all the time.
Purpura (say "PURR-pyuh-ruh" or “PURR-puh-ruh”):
- Is sudden, severe bruising that occurs for no clear reason.
- May be in one area or all over.
- Is different than the bruising that happens after you bump into something.
Symptoms of a severe allergic reaction (anaphylaxis) may include:
- The sudden appearance of raised, red areas (hives) all over the body.
- Rapid swelling of the throat, mouth, or tongue.
- Trouble breathing.
- Passing out (losing consciousness). Or you may feel very lightheaded or suddenly feel weak, confused, or restless.
A severe reaction can be life-threatening. If you have had a bad allergic reaction to a substance before and are exposed to it again, treat any symptoms as an emergency. Even if the symptoms are mild at first, they may quickly become very severe.
A baby that is extremely sick:
- May be limp and floppy like a rag doll.
- May not respond at all to being held, touched, or talked to.
- May be hard to wake up.
A baby that is sick (but not extremely sick):
- May be sleepier than usual.
- May not eat or drink as much as usual.
Many prescription and nonprescription medicines can cause a rash. A few common examples are:
- Antibiotics.
- Aspirin, ibuprofen (Advil, Motrin), and naproxen (Aleve).
- Pain medicines, such as codeine.
- Seizure medicines.
Shock is a life-threatening condition that may occur quickly after a sudden illness or injury.
Symptoms of shock in a child may include:
- Passing out (losing consciousness).
- Being very sleepy or hard to wake up.
- Not responding when being touched or talked to.
- Breathing much faster than usual.
- Acting confused. The child may not know where he or she is.
Seek Care Today
Based on your answers, you may need care soon. The problem probably will not get better without medical care.
- Call your doctor today to discuss the symptoms and arrange for care.
- If you cannot reach your doctor or you don't have one, seek care today.
- If it is evening, watch the symptoms and seek care in the morning.
- If the symptoms get worse, seek care sooner.
Seek Care Now
Based on your answers, you may need care right away. The problem is likely to get worse without medical care.
- Call your doctor now to discuss the symptoms and arrange for care.
- If you cannot reach your doctor or you don't have one, seek care in the next hour.
- You do not need to call an
ambulance unless:
- You cannot travel safely either by driving yourself or by having someone else drive you.
- You are in an area where heavy traffic or other problems may slow you down.
Make an Appointment
Based on your answers, the problem may not improve without medical care.
- Make an appointment to see your doctor in the next 1 to 2 weeks.
- If appropriate, try home treatment while you are waiting for the appointment.
- If symptoms get worse or you have any concerns, call your doctor. You may need care sooner.
Call 911 Now
Based on your answers, you need emergency care.
Call 911 or other emergency services now.
Home Treatment
Most rashes will go away without medical treatment. Home treatment can often relieve pain and itching until the rash goes away.
If your child has come in contact with a substance that may cause contact dermatitis, such as poison ivy, immediately wash the area with large amounts of water.
Once a rash has developed, leave it alone as much as possible.
- Use soap and water sparingly.
- Leave the rash exposed to the air whenever possible.
- Encourage your child not to scratch the rash.
If your child has a rash, he or she should not be in contact with other children or pregnant women. Most viral rashes are contagious, especially if a fever is present.
Relief from itching
Itching with a rash is generally not serious, but it can be annoying and may make a rash more likely to become infected. Rashes caused by chickenpox, eczema, or contact dermatitis are much more likely to itch. Sometimes itching can get worse by scratching.
Home treatment may help the itching.
- Keep your child's fingernails clean and short, and encourage him or her not to scratch. Cover your baby's hands with socks to help keep him or her from scratching.
- Keep your child out of the sun and in a cool place. Heat makes itching worse.
- Keep the itchy area cool and wet if your child is older than age 9 months. Put cloths soaked in ice water on the rash a few times a day. Too much wetting and drying will dry the skin, which can increase itching. Do not put cloths soaked in ice water on the skin of a baby younger than 9 months. It may cause the baby's body temperature to go down.
- Add a handful of oatmeal (ground to a powder) to your child's bath. Or you can try an oatmeal bath product, such as Aveeno.
- Dress your child in cotton clothing. Do not use wool and synthetic fabrics next to the skin.
- Use gentle soaps, such as Basis, Cetaphil, Dove, or Oil of Olay, and use as little soap as possible. Do not use deodorant soaps on your child.
- Wash your child's clothes with a mild soap, such as CheerFree or Ecover, rather than a detergent. Rinse twice to remove all traces of the soap. Do not use strong detergents.
- Do not let the skin become too dry, which can make itching worse.
Nonprescription medicines for itching
Carefully read and follow all label directions on the medicine bottle or box.
- Try calamine lotion for a rash caused by contact dermatitis, such as poison ivy or poison oak rashes.
- For severe itching, apply hydrocortisone cream 4 times a day until the itch is gone. Note: Do not use the cream on children younger than age 2 unless your doctor tells you to do so. Do not use in the rectal or vaginal area on children younger than age 12 unless your doctor tells you to do so.
- Try an oral antihistamine to help the scratch-itch cycle. Examples include a non-drowsy one like loratadine (Claritin) or one that might make you sleepy like diphenhydramine (Benadryl). Oral antihistamines are helpful when itching and discomfort are preventing your child from doing normal activities, such as going to school or getting to sleep. Don't give antihistamines to your child unless you've checked with the doctor first.
| Try a nonprescription medicine to help treat your child's fever or pain: |
|---|
Talk to your child's doctor before switching back and forth between doses of acetaminophen and ibuprofen. When you switch between two medicines, there is a chance your child will get too much medicine. |
| Be sure to follow these safety tips when you use a nonprescription medicine: |
|---|
|
Symptoms to watch for during home treatment
Call your child's doctor if any of the following occur during home treatment:
- Other symptoms, such as a fever, feeling ill, or signs of infection, are severe or become worse.
- A new rash lasts longer than 2 weeks.
- Your child's symptoms become more severe or more frequent.
Prevention
Several childhood diseases that cause a rash can be prevented through immunization. Immunizations help your child's immune system recognize and quickly attack a virus before it can cause a serious illness. Immunizations for chickenpox and for measles, mumps, and rubella (MMR) can prevent these common rash-causing illnesses.
Other tips for preventing rashes include the following:
- Dress your baby in as few clothes as possible during hot weather.
- Do not bathe your child too often to prevent dry skin. Most children do not need daily bathing. Children with very dry skin may do better if they bathe once or twice a week.
Preparing For Your Appointment
To prepare for your appointment, see the topic Making the Most of Your Appointment.
You can help your doctor diagnose and treat your child's condition by being prepared to answer the following questions:
- What is the history of the rash, including:
- When did the rash start?
- Where did the rash start?
- Has the rash spread?
- Has the rash changed?
- Has anything made the rash better or worse?
- Has your child had this rash before? If yes:
- What were the circumstances?
- When did he or she last have it?
- How was it treated?
- How long did it last?
- What other symptoms has your child had? Symptoms may include itching, burning, stinging, tingling, numbness, pain, tenderness to the touch, fever, cold symptoms, or diarrhea.
- Has your child been exposed to a contagious illness, such as measles, rubella, mumps, or chickenpox?
- Have you recently used a new food, medicine, or product, such as soaps, detergents, shampoos, lotions, fabrics, new toys, or other object?
- Has your child been exposed to poisonous plants, such as poison ivy, oak, or sumac?
- Has your child had other health problems during the past 3 months?
- Has your child recently traveled to a rural area or to another country?
- Does anyone in your immediate family have a skin disorder or an allergy?
- What home treatment measures have you tried? Did they help?
- What nonprescription medicines have you tried? Did they help?
- Does your child have any health risks?
Related Information
Credits
ByHealthwise Staff
Primary Medical Reviewer William H. Blahd, Jr., MD, FACEP - Emergency Medicine
Kathleen Romito, MD - Family Medicine
Specialist Medical Reviewer Adam Husney, MD - Family Medicine
Current as ofJanuary 29, 2018
- Top of Page
Next Section:
Check Your Symptoms
Previous Section:
Topic Overview- Top of Page
Next Section:
Home Treatment
Previous Section:
Check Your Symptoms- Top of Page
Next Section:
Prevention
Previous Section:
Home Treatment- Top of Page
Next Section:
Preparing For Your Appointment
Previous Section:
Prevention- Top of Page
Next Section:
Related Information
Previous Section:
Preparing For Your Appointment- Top of Page
Next Section:
Credits
Previous Section:
Related Information- Top of Page
Current as of: January 29, 2018