Juvenile Idiopathic Arthritis
Topic Overview

What is juvenile idiopathic arthritis?
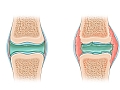
Juvenile idiopathic arthritis (JIA) is a childhood disease that causes inflamed, swollen joints. This makes joints stiff and painful. The term "juvenile idiopathic arthritis" is replacing the American "juvenile rheumatoid arthritis" and the European "juvenile chronic arthritis."
Some children with JIA grow out of it after they get treatment. Others will need ongoing treatment as adults.
There are several types of JIA.
- Oligoarticular (formerly known as pauciarticular) is the most common form. It is often the mildest type. In this type, 1 to 4 joints are affected in the first 6 months of the disease. If 4 or fewer joints continue to be affected after the first 6 months, it is called persistent oligoarthritis. If more joints become affected after 6 months, it is called extended oligoarthritis. Your child may have pain in the knees, ankles, fingers, toes, wrists, elbows, or hips.
- Polyarticular affects 5 or more joints in the first 6 months of symptoms and tends to get worse over time. It can be severe. It may be more like rheumatoid arthritis in adults.
- Systemic can be the most serious. It causes pain in many joints. It can also spread to organs.
- Enthesitis-related most often affects the areas where tendons and ligaments attach to bones (the enthesis). The joints may also be affected.
- Psoriatic usually combines joint tenderness and inflammation with psoriasis of the skin or problems with nails.
What causes JIA?
Doctors don't really know what causes the disease. But there are a number of things that they think can lead to it. These things include:
- An immune system that is too active and attacks joint tissues.
- Viruses or other infections that cause the immune system to attack joint tissues.
- Having certain genes that make the immune system more likely to attack joint tissues.
What are the symptoms?
Children can have one or many symptoms, such as:
- Joint pain.
- Joint swelling.
- Joint stiffness.
- Trouble sleeping.
- Problems walking.
- Fever.
- Rash.
In some cases these symptoms can be mild and hard for you to see. A young child may be more cranky than normal. Or a child may go back to crawling after he or she has started walking. Your child's joints may feel stiff in the morning. Or your child may have trouble walking.
Children with this disease can also get inflammatory eye disease. This can lead to permanent vision problems or blindness if it's not treated. Eye disease often has no symptoms before vision loss occurs.
How is JIA diagnosed?
Your doctor will ask questions about your child's symptoms and past health and will do a physical exam. Your child may also have blood tests and a urine test to look for signs of the disease. If your child has the disease, these tests can help your doctor find out which type it is.
How is it treated?
Your child's treatment will be based on the type of JIA he or she has, and how serious it is.
- Disease-modifying antirheumatic drugs (DMARDs) may be used to prevent the arthritis from injuring bones and joints.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) reduce pain and inflammation.
- Exercise and physical therapy help keep your child's muscles flexible and strong.
- Occupational therapy helps your child live as independently as possible.
- Surgery to correct joint problems is only done in rare cases.
Even when JIA isn't severe, your child may still need long-term treatment. To make sure that treatment is right for your child, work closely with the medical team. Learn as much as you can about your child's disease and treatments. Stay on a schedule with your child's medicines and exercise.
How do you cope with JIA?
Take good physical care of yourself so that you can help your child through the more difficult periods of illness. Consider finding a support group of families who live with juvenile idiopathic arthritis. Your local chapter of the Arthritis Foundation can provide classes and support group information.
Frequently Asked Questions
Learning about juvenile idiopathic arthritis: | |
Being diagnosed: | |
Getting treatment: | |
Ongoing concerns: |
Cause
The cause of juvenile idiopathic arthritis (JIA) isn't well understood. Most experts believe it is caused by a combination of things, including:
- An immune system that is too active and attacks joint tissues.
- Viruses or other infections that cause the immune system to attack joint tissues.
- Having certain genes that make the immune system more likely to attack joint tissues.
Symptoms
The most common symptoms of all forms of juvenile idiopathic arthritis (JIA) include:
- Joint pain and swelling. They may come and go, but they are most often persistent.
- Joint stiffness in the morning.
- Irritability, refusal to walk, or protecting or guarding a joint. You might notice your child limping or trying not to use a certain joint.
- Often unpredictable changes in symptoms, from periods with no symptoms (remission) to flare-ups.
Even though pain is a common symptom of JIA, your child may not be able to describe the pain. Or he or she may be used to the pain. To know if your child is in pain, look for changes such as stiff movements, rubbing a joint or muscle, or avoiding movement.
Other symptoms vary depending on which type of JIA your child has.
Systemic JIA can cause fever spikes and rash.
- The fever usually reaches 103°F (39.5°C) to 106°F (41°C) once or twice a day. It falls to normal between spikes.
- The rash is spotty, flat, and sometimes faint red or pink. It may occur with the fever. It may be on the torso, face, palms, soles of the feet, and armpits. The rash often comes and goes. It may appear late in the day or in the early morning. It may also be brought on by warm baths or by rubbing or scratching the skin.
Other conditions with symptoms similar to JIA include growing pains, overuse, injury, bone infection, and certain inflammatory diseases. Many conditions can cause painful, stiff joints in children. Most often, occasional joint pain in children is related to an injury or aggravating factors, such as repetitive overuse in sports activities. JIA is a fairly uncommon cause of these symptoms.
What Happens
The course of juvenile idiopathic arthritis (JIA) is unpredictable, especially during the first few years after a child is diagnosed. JIA can be mild, causing few problems. It can get worse or disappear without clear reason. Over time, the pattern of symptoms becomes more predictable. Most children have good and bad days.
Of all children who have JIA, 3 or 4 out of 10 children will have long-term disability.footnote 1 Long-term disability may range from occasional stiffness, the need for pain medicine, and limits on physical activity to ongoing JIA and the need for major surgery such as joint replacement. But for most adults who had JIA as children, any long-term problems tend to be mild and don't affect their overall quality of life.
A child's long-term outlook depends on the type of JIA and any complications he or she has. Treatment also affects the child's long-term outlook. Starting treatment early may help lower the chance of long-term disability.
Types of JIA
- Oligoarticular JIA (oligoarthritis): Oligoarticular (formerly known as pauciarticular) is the most common form of JIA. It is often the mildest type. In this type, 1 to 4 joints are affected in the first 6 months of the disease. If 4 or fewer joints continue to be affected after the first 6 months, it is called persistent oligoarthritis. If more joints become affected after 6 months, it is called extended oligoarthritis. Your child may have pain in the knees, ankles, fingers, toes, wrists, elbows, or hips. He or she may continue to have the disease as an adult. This risk is higher if more joints are affected after the first 6 months.
- Polyarticular JIA (polyarthritis): Polyarticular JIA affects 5 or more joints in the first 6 months of symptoms. This type of JIA is more severe than most cases of oligoarticular JIA. That's because polyarticular JIA affects more joints, and it tends to get worse over time. Many children will have active disease that continues into adulthood. There are two types: rheumatoid factor-positive (RF-positive) and rheumatoid factor-negative (RF-negative).
- Systemic JIA: Systemic can be the most serious. It causes pain in many joints. It can also spread to organs. Many will continue to have active disease as adults. While some children have one course of this disease that lasts 2 to 4 years, others continue to have mild joint pain and flares of other symptoms. A few have ongoing destructive arthritis, often into adulthood, even with treatment.
- Enthesitis-related JIA: Enthesitis-related most often affects the areas where tendons and ligaments attach to bones (the enthesis). The joints may also be affected. The long-term outlook for this form of JIA is less well known. Some children progress to other conditions such as adult ankylosing spondylitis. This is more common in boys who have hip arthritis.
- Psoriatic JIA: Psoriatic is the least common form of JIA. Children with psoriatic arthritis usually have joint tenderness and inflammation combined with psoriasis of the skin or problems with nails. The long-term outcome for this type of JIA isn't well known. Some children continue to have skin and joint symptoms. For a few, the ability to do daily activities can become limited.
Learn more about the symptoms and what happens in the types of JIA.
Complications
Complications associated with JIA can include:
- Inflammatory eye disease, such as uveitis. Children and adults with this condition can develop cataracts, glaucoma, corneal degeneration (band keratopathy), or vision loss.
- Growth abnormalities. These include unequal leg lengths, an imbalance in growth of the jaw, and temporary delay in breast growth.
- Joint damage, including changes in the cartilage and other tissues that line the inside of the joints, and changes to the bones themselves.
Some children with polyarthritis get arthritis in the neck that can cause the neck bones to fuse together.
Complications of systemic JIA include heart or lung problems, such as pericarditis, pleuritis, or pericardial effusion. A rare lung complication is the formation of scar tissue in the lungs (pulmonary fibrosis).
What Increases Your Risk
No clear risk factors for juvenile idiopathic arthritis (JIA) are known at this time. It may run in families.
When To Call a Doctor
Call your doctor immediately if:
- Your child has sudden, unexplained swelling, redness, and pain in any joint or joints.
- A baby or child is unusually cranky or reluctant to crawl or walk.
- Red eyes, eye pain, and blurring or loss of vision occur in a child who has been diagnosed with any form of juvenile arthritis.
Call your doctor if any of the following symptoms continue for more than 2 days:
- A child has unexplained daily fever spikes [103°F (39.4°C) to 106°F (41.1°C)] with or without a pink skin rash.
- A baby or child is reluctant to crawl or walk in the early morning but improves after 1 to 2 hours.
- A child taking aspirin or another nonsteroidal anti-inflammatory drug (NSAID) develops stomach pain not clearly related to stomach flu, but possibly related to medicine use. (Symptoms may include heartburn, nausea, or refusal to eat.)
- Joint pain and skin rash develop following a sore throat.
It can be hard to know when an infant has joint pain. A young child may be unusually cranky or may revert to crawling after he or she has started walking. You may notice gait problems with a walking child or stiffness in the morning.
Who to see
For a first check of joint pain and other symptoms of juvenile idiopathic arthritis (JIA), consult with a:
For more testing and disease management, consult with a rheumatologist who specializes in children's rheumatic disease (pediatric rheumatologist).
The disease management team for JIA may also include:
- An orthopedic surgeon who specializes in children's orthopedic problems (pediatric orthopedist).
- Nurses.
- Physical and occupational therapists.
- A registered dietitian, as needed.
- A social worker or psychologist, as needed.
- A general dentist and an orthodontist, as needed.
- An ophthalmologist.
To prepare for your appointment, see the topic Making the Most of Your Appointment.
Exams and Tests
Findings from a physical exam, including the pattern and nature of joint symptoms, are important keys to the diagnosis of juvenile idiopathic arthritis (JIA). Lab tests may be used to support the diagnosis and make sure symptoms aren't caused by another health problem. JIA is often diagnosed only after other possible causes of symptoms have been ruled out and the pain and stiffness have lasted for at least 6 weeks.
Routine exams and tests include the following:
- Medical history and physical exam
- Complete blood count (CBC)
- Erythrocyte sedimentation rate (ESR, or sed rate)
- Urinalysis
- Rapid strep test or throat culture (to test for strep throat)
The following tests are done if needed:
- Rheumatoid factor (RF), to clarify whether a child with polyarticular JIA is RF-positive or RF-negative
- Antinuclear antibody (ANA), to clarify a child's type of JIA and risk for eye disease
- X-ray of joints
- An MRI scan, which may reveal early joint damage
- HLA-B27 genetic test
Your doctor will probably schedule routine checkups to see how your child is doing and how well treatment is working. This will include talking about inflammatory eye disease and exams for this disease, such as a slit lamp eye exam.
Treatment Overview
Treatment goals for juvenile idiopathic arthritis (JIA) are to reduce your child's joint pain and to prevent disability. Physical therapy and medicine are the basis of medical treatment for JIA.
Treatment depends on the type and severity of JIA. Even when JIA is uncomplicated, an affected child may need years of medical treatment or checkups. To make sure that your child's care is appropriate for the stage of disease, work closely with the medical team. Learn as much as you can about your child's disease and treatments. And stay on schedule with medicine and exercise.
Your doctor will set up a treatment team. It may include a pediatrician, an ophthalmologist, a rheumatologist, and a physical and/or occupational therapist.
Physical therapy
Treatment may include:
- Physical therapy. Regular exercise and range-of-motion exercises will help maintain joint range and muscle strength and prevent contractures.
- Occupational therapy. An occupational therapist (OT) can help your child learn ways to do self-care activities, play, and take part in school without making symptoms worse.
- Balancing rest and activity. Mix extra naps or quiet times with activity each day.
- Assistive devices. These can help your child hold onto, open, close, move, or do things more easily.
- A pain management plan. This can help you and your child control pain caused by JIA.
To learn more, see Home Treatment and Other Treatment.
Medicines
Medicine will likely be an important part of your child's treatment.
- Disease-modifying antirheumatic drugs (DMARDs) may be used to prevent the arthritis from injuring bones and joints.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) are used to reduce inflammation and pain.
- A corticosteroid injection into a joint also may be used to reduce inflammation, particularly if your child has oligoarticular JIA.
- Combinations of medicines may also be used.
To learn more, see Medications.
Follow-up
Treatment depends on the type and severity of JIA. Even when JIA is uncomplicated, an affected child may need years of medical treatment or checkups. To make sure that your child's care is appropriate for the stage of disease, work closely with the medical team. Learn as much as you can about your child's disease and treatments. And stay on schedule with medicine and exercise.
Inflammatory eye disease may develop in children with JIA. This form of eye disease generally has no symptoms and can lead to a permanent decrease in vision or blindness. So part of your child's treatment plan should be regular checkups with an ophthalmologist.
What to think about
Surgery may be used in a very small number of children with JIA who have severe joint deformity, loss of movement, or pain.
Some children with JIA have no appetite, so malnutrition becomes a medical concern. If your child has little appetite for food, see a registered dietitian for help.
Prevention
The cause of juvenile idiopathic arthritis (JIA) isn't well understood, and there is no way to prevent it. But you can help prevent symptoms. See Home Treatment.
Home Treatment
You can do a lot at home to help your child lead a normal life, relieve his or her symptoms, and prevent complications.
- Do range-of-motion exercises. These help maintain your child's joint range and muscle strength. They also prevent contractures. You may need to help an infant or younger child do the exercises.
- Find a balance between rest and activity. Your child may need extra naps or quiet time to rest the joints and regain strength. But too much rest may lead to weakness in unused muscles.
- Partner with school staff. You can plan creative ways of dealing with JIA-caused limitations. This can help your child make the best of his or her abilities.
- Stick to a medicine schedule. An older child may find it easier to remember to take medicine by using a pillbox or chart for a day's or week's worth of medicine. Ask your doctor if the dosage can be adjusted so your child can take it at times that are most convenient and won't make him or her feel "different." To avoid stomach upset, you can also give nonsteroidal anti-inflammatory drugs (NSAIDs) with meals or a small snack. Be safe with medicines. Read and follow all instructions on the label.
- Use assistive devices. These can help your child hold on to, open, close, move, or do things more easily. Devices include Velcro fasteners and enlarged handles. Getting your child lightweight clothing and toys will also help.
- Make sure your child sees the doctor regularly. He or she should also have eye exams with an ophthalmologist. Inflammatory eye disease can develop as a complication in children with JIA.
Dealing with stiffness
- Apply heat to stiff and painful joints for 20 minutes, repeating as needed. You can use hot water bottles. Or make hot packs from towels dipped in warm water or wet towels microwaved for 15 to 30 seconds. Always make sure that hot water bottles and hot packs aren't too hot for your child's skin. Keep a cloth between the hot water bottle and your child's skin. Do not use heat if your child's joints are red and warm.
- Many children who have JIA have less stiffness in the morning if their joints are kept warm during the night. To help keep joints warm, try footed pajamas, thermal underwear, a sleeping bag, a heated water bed, or an electric blanket.
- Encourage your child to take a warm bath or shower first thing in the morning. It can help ease stiffness. Have your child stretch gently afterward.
- Give morning medicines as early as possible, with a snack or breakfast, to prevent upsetting an empty stomach.
Help yourself to help your child
Living with JIA often means making lifestyle changes and adjustments. This can be frustrating and demanding for you, your child, and your family. Here are a few steps to help yourself:
- Learn about the disease. Knowing more about it will help you and your child have less fear, make better decisions, and have better results.
- Work as a team with your child's doctors and other health professionals. The outlook is better when you and your child actively manage your child's health.
- Take good physical care of yourself so that you can help your child through the more difficult periods of illness. Consider becoming involved with a support group of families who live with JIA. Your local chapter of the Arthritis Foundation can provide classes and support-group information.
- Remember that many children with JIA don't have long-term disease and disability. They go on to lead healthy adult lives.
Medications
Most children with juvenile idiopathic arthritis (JIA) need to take medicine to reduce inflammation and control pain and to help prevent more damage to the joints. When inflammation and pain are controlled, a child is more willing and able to do joint exercises to improve joint strength and prevent loss of movement.
Many different medicines are used to treat JIA. No single medicine works for every child. Your doctor will try to find medicine that helps relieve symptoms and that has few side effects. This may take some time.
Medicine choices
Treatment varies depending on the needs of each child, but certain medicines are often tried first. These medicines include those that modify the disease and some to help relieve pain. Be safe with medicines. Read and follow all instructions on the label.
Medicines to treat JIA
- Disease-modifying antirheumatic drugs (DMARDs), also called slow-acting antirheumatic drugs (SAARDs), include:
- Methotrexate.
- Sulfasalazine.
- Biologics such as adalimumab, etanercept, or tocilizumab.
- Nonsteroidal anti-inflammatory drugs (NSAIDs). NSAIDs reduce inflammation and pain, especially before DMARDs can take effect. Naproxen is the most often used NSAID treatment for JIA because of its low incidence of side effects compared to its effectiveness. Ibuprofen may be used instead. But in general, less than one-third of children will have significant relief from NSAIDs.footnote 1 If you see no improvement after 6 weeks, your doctor may try a different NSAID.
- Corticosteroids. Injections can be used for children who have just a few joints affected or who have enthesitis. Steroid medicines by mouth or through an IV are often used for widespread joint pain or systemic problems such as fever or pericarditis. Steroid medicines work faster than some other drugs, so they may also be used until other medicines start working. Corticosteroids are sometimes used with disease-modifying antirheumatic drugs (DMARDs).
- Antimalarials, such as hydroxychloroquine.
- Other therapies, such as cytotoxic (cell-destroying) drugs and intravenous human immunoglobulin.
Medicines to treat inflammatory eye disease
- Corticosteroid eyedrops
- DMARDs, such as adalimumab.
- Mydriatics, which are eyedrops that dilate the pupil and keep the iris from sticking to the cornea or lens
If your child is on aspirin therapy
Yearly flu shots are recommended for children who are on long-term aspirin therapy. Children on long-term aspirin therapy who get chickenpox or the flu are at risk for getting Reye syndrome. Although there is a risk, Reye syndrome is very rare. Very few cases have been reported in children with chronic arthritis who were being treated with aspirin. If your child has been exposed to chickenpox or the flu, talk to the doctor about giving your child acetaminophen to control pain and relieve fever until the incubation period, or the illness itself, has passed.
Surgery
Surgical treatment may be used in a very small number of children whose juvenile idiopathic arthritis (JIA) has caused severe joint deformity, loss of movement, or pain.
The main things to think about for surgery during childhood are the child's age and whether his or her bones are still growing. If at all possible, joint reconstruction is delayed until childhood bone growth is complete (at about 18 years of age).
Surgery choices
When surgery to correct joint deformity is needed, the more common procedures include:
- Soft tissue releases of contractures. This involves cutting the muscles attached to an abnormally bent joint.
- Total joint replacement. Important things to consider include your child's age, the number of joints involved in the disease, and the impact on your child's mobility.
Other surgical procedures for JIA are recommended only in selected cases. These include:
- Osteotomy, which involves removing a wedge of bone to allow more normal alignment of the joint. It may be recommended for children who have severe joint contractures.
- Epiphysiodesis. In this surgery, the portion where growth occurs is removed in order to stop growth.
- Synovectomy or tenosynovectomy. These are rarely used for JIA. Synovectomy involves the removal of the joint lining (synovium) and/or the covering of the tendon (tenosynovectomy) to reduce joint inflammation.
- Arthrodesis. This is rarely used in children. It involves fusing two bones in a diseased joint so that the joint can no longer move.
Other Treatment
Other treatment for juvenile idiopathic arthritis (JIA) includes physical and occupational therapy, healthy eating, pain management, and some complementary therapies.
Physical and occupational therapy
Physical therapy will be an important part of treatment if your child has severe JIA. The physical therapist can help set up an exercise program for your child, either for the child to do alone or to do with help from an adult. Exercises should be done every day and should be regularly reviewed by the physical therapist. The therapist will make sure that the exercises are being done correctly. He or she can decide whether any exercises should be added, dropped, or changed.
Occupational therapy helps a child live as independently as possible.
Any of the following may be used in physical or occupational therapy:
- Physical conditioning. It may include aerobic exercise, range-of-motion exercises, and strength and stretching exercises.
- Stretching and strengthening exercises. They can help a child maintain strength and a normal range of motion.
- Splinting at night. Splinting will help keep the wrist, hand, knee, and/or ankle joints straight. This may prevent pain, morning stiffness, and contractures. Working splints can help support a joint and relieve pain during writing or other hand tasks.
- Serial casting of the knees, ankles, wrists, fingers, and/or elbows. This is a temporary straightening and casting of the affected joint. The cast is then removed, and the child goes through some physical therapy. Then a new cast is applied with the joint stretched a bit more.
- Shoe lifts or inserts. These help to equalize leg lengths for children in whom one leg grows at a different rate than the other. For some types of inflammation in the feet, you can try using shoe inserts that transfer your weight onto your heel. This takes weight off the sore middle or front part of the foot.
Healthy eating
Healthy eating means eating a variety of foods so that your child gets the nutrients he or she needs for growth and development. Good nutrition may also help fight the effects of JIA. Your child can eat all types of food as long as his or her weekly intake is balanced and varied.
Talk to your child's doctor about healthy foods for children with JIA. There are a few nutrients that may be helpful. These include:
- Vitamin D and calcium, which can help control bone loss that is often linked with inactivity and with corticosteroid treatment.
- Vitamin C, which is an antioxidant that may help reduce inflammation in the body. It is found in citrus fruits, tomatoes, berries, broccoli, cabbage, and brussels sprouts.
- Omega-3 fatty acids in fish oil, which have been shown to mildly reduce inflammation in adults with rheumatoid arthritis. They may have the same effect in children who have JIA. Good sources of omega-3 fatty acids are cold-water fish and flaxseed oil.
Pain management
- A pain management plan can help you and your child control pain caused by JIA.
- Heat, cold, or water therapy may reduce muscle spasms around joints, which can cause significant pain and movement problems.
Complementary medicine therapies for pain management
- Massage is used to promote relaxation, relieve pain, and restore normal joint movement.
- Guided imagery may be used to promote relaxation and manage pain.
- Acupuncture is mildly effective in relieving pain in adults who have rheumatoid arthritis. It may help relieve pain in children who have JIA, but this has not been proved.
Other Places To Get Help
Organizations
References
Citations
- Hashkes PJ, Laxer RM (2005). Medical treatment of juvenile ideopathic arthritis. JAMA, 294(13): 1671-1684.
Other Works Consulted
- Duffy CM, et al. (2005). Nomenclature and classification in chronic childhood arthritis. Arthritis and Rheumatism, 52(2): 382-385.
- Goldmuntz EA, White PH (2006). Juvenile idiopathic arthritis: A review for pediatricians. Pediatrics in Review, 27(4): e24-e32.
- Gomez FE, Kaufer-Horwitz M (2012). Medical nutrition therapy for rheumatic disease. In LK Mahan et al., eds., Krause's Food and the Nutrition Care Process, 13th ed., pp. 901-922. St Louis: Saunders.
- Hsu JJ, et al. (2013). Treatment of juvenile idiopathic arthritis. In GS Firestein et al., eds., Kelley's Textbook of Rheumatology, 9th ed., vol. 2, pp. 1752-1770. Philadelphia: Saunders.
- Petty RE, et al. (2004). International League of Associations for Rheumatology classification of juvenile idiopathic arthritis: Aecond revision, Edmonton, 2001. Journal of Rheumatology, 31(2): 390-392.
- Ringold S, et al. (2013). 2013 update of the 2011 American College of Rheumatology recommendations for the treatment of juvenile idiopathic arthritis: Recommendations for the medical therapy of children with systemic juvenile idiopathic arthritis and tuberculosis screening among children receiving biologic medications. Arthritis Care and Research, 65(10): 1551-1563. DOI: 10.1002/art.38092. Accessed February 5, 2015.
- Simon L, et al. (2002). Treatment of pain in children and older adults with arthritis. In Guideline for the Management of Pain in Osteoarthritis, Rheumatoid Arthritis, and Juvenile Chronic Arthritis, 2nd ed., chap. 5, pp. 119-129. Glenview, IL: American Pain Society.
- Wedderburn LR, Nistala K. (2013). Etiology and pathogenesis of juvenile idiopathic arthritis. In GS Firestein et al., eds., Kelley's Textbook of Rheumatology, 9th ed., vol. 2, pp. 1741-1751. Philadelphia: Saunders.
- Wilson D, Curry M (2011). The child with musculoskeletal or articular dysfunction. In MJ Hockenberry, D Wilson, eds., Wong's Nursing Care of Infants and Children, 9th ed., pp. 1619-1688. St. Louis, MO: Mosby Elsevier.
Credits
ByHealthwise Staff
Primary Medical Reviewer Susan C. Kim, MD - Pediatrics
E. Gregory Thompson, MD - Internal Medicine
Martin J. Gabica, MD - Family Medicine
Kathleen Romito, MD - Family Medicine
Specialist Medical Reviewer John Pope, MD - Pediatrics
Current as ofJanuary 24, 2018
- Top of Page
Next Section:
Cause
Previous Section:
Topic Overview- Top of Page
Next Section:
Symptoms
Previous Section:
Cause- Top of Page
Next Section:
What Happens
Previous Section:
Symptoms- Top of Page
Next Section:
What Increases Your Risk
Previous Section:
What Happens- Top of Page
Next Section:
When To Call a Doctor
Previous Section:
What Increases Your Risk- Top of Page
Next Section:
Exams and Tests
Previous Section:
When To Call a Doctor- Top of Page
Next Section:
Treatment Overview
Previous Section:
Exams and Tests- Top of Page
Next Section:
Prevention
Previous Section:
Treatment Overview- Top of Page
Next Section:
Home Treatment
Previous Section:
Prevention- Top of Page
Next Section:
Medications
Previous Section:
Home Treatment- Top of Page
Next Section:
Surgery
Previous Section:
Medications- Top of Page
Next Section:
Other Treatment
Previous Section:
Surgery- Top of Page
Next Section:
Other Places To Get Help
Previous Section:
Other Treatment- Top of Page
Next Section:
References
Previous Section:
Other Places To Get Help- Top of Page
Next Section:
Credits
Previous Section:
References- Top of Page
Current as of: January 24, 2018